If you are living with Parkinson’s, you likely know that it has become the fastest growing neurological condition in the world. You likely know that many treatment options exist, from medication to exercise, surgical options, complementary therapies, and more. You likely know that clinical trials and research continue to explore innovative new strategies for managing symptoms and, ideally, slowing or even stopping the progression of Parkinson’s. But, even knowing all of this, it can be difficult to know when, and how, you should consider a different Parkinson’s medication. In this post, we offer answers to these common questions.
An Array of Medication Options
Although carbidopa/levodopa remains the gold standard of Parkinson’s medications, there are new drugs and other interventions being investigated, approved, and incorporated into Parkinson’s treatment regimens all the time. This is positive in countless ways. Because everyone experiences Parkinson’s differently, everyone responds to medications differently, so, having many options available is critical. And because Parkinson’s progresses and changes over time, having many options available can help you tailor your treatment to the symptoms that are most burdensome to you at a particular time. (For an in-depth look at all the options currently available for treating Parkinson’s motor symptoms, be sure to check out this webinar with movement disorder specialist Dr. Aaron Haug.)
When to Consider a Different Parkinson’s Medication
As Dr. Haug often says, the best time to begin Parkinson’s medications is when your symptoms begin to negatively impact your quality of life. The same is true when it comes to considering a new treatment plan. If the medications you have been taking are no longer managing your symptoms, as often happens after you’ve been living with Parkinson’s for several years, it’s time to talk to your physician about different options.
When a person has lived with Parkinson’s for more years, they usually need more treatment. The medicine doesn’t stop working, but progression of Parkinson’s leads to more symptoms. There are multiple ways to address this, including increasing the dose of one medicine, or using multiple medicines together. The guiding principle is to start medication if symptoms are negatively impacting you and adjust medications over time to maximize quality of life.
-Dr. Aaron Haug, MD
Here are some good reasons to consider new or different medications:
- You are experiencing more OFF times when your medications aren’t working optimally, and your symptoms return
- You notice symptom fluctuations that haven’t occurred before
- You begin experiencing side effects from your Parkinson’s medications that are lowering your quality of life
- You begin experiencing new motor or non-motor symptoms
Even if your medication is working well, you may need to consider a different treatment if your drug moves to an exclusion list, meaning it is no longer covered by your insurance plan. If this happens to a medication you’re taking, there are several important steps to take (see this article to learn more). If one of these steps includes switching drugs, be sure to work closely with your physician to titrate off your current medication to avoid bothersome and sometimes very dangerous side effects.
Finally, you may wish to talk with your physician about new medications and/or other interventions because you’ve heard from advertisements, friends, support group members, or other members of your care team that a new Parkinson’s drug or therapy may work well for you. With all the new branded treatments on the market, it makes good sense to research the options and talk with your physician about what is available to you.
How to Consider Different Parkinson’s Medications
Now, let’s look at how you can explore different Parkinson’s medications.
Please remember that it’s never okay to change strategies without consulting with your doctors.
Strategy: Increase the Dose of One Medication
As Parkinson’s progresses, your brain produces less and less dopamine, so, it must rely much more heavily on levodopa or other drugs to control your symptoms. You may begin to experience fewer benefits from your medication and feel OFF more often. For some people, simply increasing the dosage of carbidopa/levodopa, a dopamine agonist, or another Parkinson’s medication can help. Whereas in the past you might have experienced symptom relief from one or two daily doses, you may now need three or more in order to minimize ON/OFF fluctuations. For some people with Parkinson’s, increasing doses may be the only medication-adjustment step they need to take for several years.
Strategy: Incorporate New Medications into Your Drug Regimen
If you have already taken the step of increasing the doses of your medication, but it’s not working, it’s time to consider exploring other options, such as adding a new drug to your regimen.

One common reason new medications are added to a Parkinson’s treatment plan is due to Parkinson’s-related dyskinesia. In Parkinson’s, dyskinesia (uncontrolled, irregular jerking, dance-like, or wriggling movements) is typically the result of increasing doses of levodopa as more is needed to compensate for dopamine loss. If your dyskinesia is interfering with your daily activities, talk with your physician about treatment options, such as adding a booster (such as MAO-B Inhibitors, COMT Inhibitors, and Adenosine-A2A Receptor Antagonists) or an extended-release medication (more on that below) that can help.
Strategy: Change Your Medication Delivery System
Extended-release medications
Extended-release medications can help manage Parkinson’s symptoms by providing a more constant level of levodopa in the bloodstream and the brain. In clinical studies, the extended-release carbidopa/levodopa drug Rytary® demonstrated a two-times reduction in OFF time during waking hours. For some people, simply switching from standard release to extended-release levodopa can dramatically improve their quality of life. Others find that using an extended-release medication like Rytary as their base treatment and taking additional medications that interact well with it is the key to managing symptoms.
If dyskinesia is a problem, talk with your physician about the extended-release formulation of amantadine (GOCOVRI®), which has been approved by the FDA to treat levodopa-induced dyskinesia in people with Parkinson’s as well as OFF. Another option is to consider other forms of amantadine, which are approved to treat Parkinson’s and may be prescribed off-label to treat dyskinesia.
Other treatment options that can help via extended delivery include the rotigotine patch, extended-release pramipexole, and extended-release ropinerole. Talk with your physician about the pros and cons of these kinds of treatment options.
Continuous release delivery systems
Continuous dopamine stimulation (CDS) is a medication delivery system that may reduce the risk of dramatic ON/OFF fluctuations and help improve or maintain quality of life as Parkinson’s progresses. The goal of CDS is to help the brain maintain more constant levels of dopamine; it does this by imitating the brain’s normal continuous pattern of stimulating dopamine receptors and keeping dopamine levels more constant over a 24-hour period.
One example of CDS is subcutaneous apomorphine infusion. During this procedure, apomorphine is administered through a portable, battery-powered mini-pump that injects the medication under your skin, usually into your abdomen. Open-label studies have shown that apomorphine infusion effectively reduces OFF times, and results from a 2018 randomized, placebo-controlled, double-blind, multicenter trial showed that apomorphine infusion resulted in a clinically meaningful reduction in OFF periods for people with Parkinson’s who experienced persistent motor fluctuations.
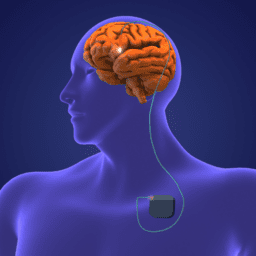
Surgical CDS options include deep brain stimulation (DBS) and enteral suspension of carbidopa/levodopa. DBS is a Parkinson’s surgical therapy in which electrodes are implanted into specific regions of the brain. These electrodes emit continuous electrical impulses (stimulation) from a stimulator device, which typically leads to improvements in many Parkinson’s motor symptoms such as tremor, stiffness, and slowness. In continuous carbidopa/levodopa enteral suspension, a carbidopa/levodopa gel suspension is delivered through a surgically implanted tube directly into the small intestine, where the medication is absorbed. The small pump, which you carry or wear, allows infusion of a constant medication dose over 16 hours each day, with your physician’s ability to prescribe additional doses at certain times.

The key to finding the best medication regimen for you is knowing when to talk to your physician about new treatments and how various treatment strategies work. Stay in-the-know about the latest medications and other interventions and go to all medical appointments with a plan to discuss options that you think might work well for you. Parkinson’s treatments are ever-changing and always improving; so, make the most of this and work with your care team to explore how various treatments can help you can live well with Parkinson’s today and every day.
This post was written by the Davis Phinney Foundation.
This blog series is sponsored by Amneal.