Everyone knows what it means to feel off, to feel like something’s just not quite right. But if you’re living with Parkinson’s, OFF times can be debilitating. The good news is that although many people with Parkinson’s believe that frequent OFF periods are an inescapable part of the experience, there are strategies you can use to minimize, or even prevent, being OFF. In this post, we’ll show you how.
What does it mean to be OFF?
The state of being OFF is when your Parkinson’s medications aren’t working optimally, and your motor and non-motor symptoms aren’t under control. OFF times look different for everyone. For some people with Parkinson’s, OFF means experiencing reduced mobility, increased tremor, muscle cramping, rigidity, slowness, balance issues, stiffness, shortness of breath, and/or swallowing issues. Feeling OFF may also worsen non-motor symptoms and cause fluctuations in cognition, attention, anxiety, depression, and apathy. OFF can also cause a person with Parkinson’s to experience increased sweating, lightheadedness, abdominal pain, bloating, urinary issues, visual disturbances, pain, dysesthesia, akathisia, and/or restless legs syndrome.
There are four types of OFF that people with Parkinson’s experience:
- Delayed ON. This is what happens when it takes a long time for your medication to kick in. It can happen with your first pill after a long night of sleep, but it can also happen later in the day if you don’t time your meals or macronutrients optimally.
- Wearing OFF. This is what happens when your medication wears off before it’s time to take your next dose. This happens more frequently as your Parkinson’s progresses.
- Unpredictable OFF. This is when your symptoms return unexpectedly, even if you take every dose as scheduled.
- Dose Failure/Partial ON. This happens when symptoms subside after taking your medication, but your meds aren’t as effective as they usually are.
Your unique OFF experience
Just like your Parkinson’s symptoms are unique to you, your OFF times are as well. Some people equate OFF times to times when motor symptoms re-emerge, and they discount the non-motor symptoms that tend to be present more often than not during OFF times. So, they’re OFF, but they don’t realize it. Some people with Parkinson’s experience an increase in motor symptoms and believe it’s caused by the progression of Parkinson’s rather than a result of their medication wearing off. They think, therefore, that there’s nothing they can do about it. Some may choose not to share any discomfort they’re having with their care partners, friends, and/or healthcare providers because they don’t want to be a burden or seem like they’re complaining. And, while some people may feel uncomfortable during OFF times, they fail to share their symptoms with anyone because they think it might be a sign that their Parkinson’s is progressing, and they aren’t ready to face that. Refusing to talk about it, in this case, serves as a coping mechanism.
How to determine when you’re ON and OFF
The first step to minimizing OFF times is to learn about the full spectrum of OFF symptoms and to track your motor and non-motor symptoms throughout the day. Pay close attention to how you feel before and after each dose of medication and ask yourself these questions:
- Do I consistently feel ON within an hour of taking my meds?
- Does this change depending on the time of day?
- Does my medication wear off more quickly in the evening?
- Does what I eat impact my ON/OFF times? How?
 Keep a diary of your daily medication schedule and use it to track your symptoms. Be as detailed as possible with times, doses, symptom onset or relief, etc. If you have a care partner who lives with you, ask them to keep a log of this information also, as they may notice the onset of symptoms that you don’t.
Keep a diary of your daily medication schedule and use it to track your symptoms. Be as detailed as possible with times, doses, symptom onset or relief, etc. If you have a care partner who lives with you, ask them to keep a log of this information also, as they may notice the onset of symptoms that you don’t.
To make this process easier, you can download our fillable symptom tracker here and our fillable OFF tracker here. At each medical appointment, take your completed worksheets and/or diaries with you to help illustrate to your healthcare providers the ON/OFF fluctuations you’re experiencing.
How to talk to your physician about ON/OFF periods
Even after you’ve taken time to notice, assess, and track what OFF feels like to you, communicating about your unique OFF experiences can still be challenging. One strategy to help is, as we explained above, taking a written tracker of your medication doses and symptom fluctuations throughout the day to all your physician appointments.
Another strategy is to have your care partner go with you to your appointments so your physician can get the full story—the one experienced by you as the person with Parkinson’s and the one observed by your care partner.
Be proactive and speak up about your symptoms and any ON/OFF fluctuations you experience at all appointments. Never assume that your physician can guess what your symptoms are or that you even have them. Your appointment time with your doctor is limited, and unless they prompt you to discuss OFF in a specific way, you may miss some key information about your medication and how it is supposed to work. Take these questions with you the next time you go to get the conversation about OFF started.
- How long should it take my medication to start working?
- Should my medication be working the same throughout the day?
- What should I do if my medication begins to wear OFF before my next dose?
- What if I take a dose and nothing happens?
- Can I take my medication when OFF symptoms occur, even if it’s not time for my next dose?
It’s also critical that you and your physician come to a standard definition of OFF. Your doctor might not think that predictably wearing off is equivalent to an OFF state. You might think it is. To account for differences in how you each define OFF, it’s important to determine what OFF means to both of you and to come up with a working definition together. You might even have a code such as, “When I say X, I mean Y.” The earlier you can establish a language for how you talk about OFF, the better chance you have of getting the interventions and treatment you need to live well with Parkinson’s.
How nutrition and GI health can help minimize OFF times
Another important step in minimizing OFF is to understand what causes it to begin with. When you understand the science behind Parkinson’s OFF, you can use this knowledge to your advantage and get the most out of your Parkinson’s medications.
 When it comes to nutrition, three key aspects to keep in mind are hydration, protein, and fiber.
When it comes to nutrition, three key aspects to keep in mind are hydration, protein, and fiber.
Hydration
For your levodopa to make its way from your mouth to your brain, it must travel from your mouth to your stomach to your small intestine, then to your blood-brain barrier, then to your brain. There, the levodopa is metabolized to produce dopamine. The more quickly levodopa reaches the small intestine, the faster it passes through the intestinal walls, the faster it reaches your brain, the faster it’s converted to dopamine, and the faster you feel ON. The longer levodopa stays in your stomach, the longer you may feel OFF.
One key strategy for preventing delayed and partial ON times is to take your levodopa on an empty stomach with a full glass of water. The water “flushes” the medicine quickly to the small intestine, and the absence of food in your stomach means nothing can slow its emptying. (Crushing or chewing carbidopa/levodopa can also help speed the process, as can drinking sparkling water or seltzer.)
Drinking enough water also helps minimize OFF times by minimizing constipation. Soluble fiber absorbs water, which helps bulk up your stool while also transforming the soluble fiber into a gel-like substance. This softens the stool and allows it to move more smoothly through your bowels. However, if your body isn’t adequately hydrated, it will soak up the water it needs from your food waste in the large intestine. This, in turn, creates hard stools that are difficult to pass. In general, you should aim to drink at least 64 ounces of water each day but talk to your physician to determine if those recommendations are suitable for you.
Protein
Have you ever noticed that when you take your carbidopa/levodopa with a protein-heavy meal, it seems less impactful on your symptoms? That’s because the amino acids in dietary protein compete with levodopa for absorption—both through the intestinal wall and then across the blood-brain barrier. If amino acids are present when levodopa is working its way through the walls of the small intestine to the bloodstream, and/or when levodopa makes its way to the blood-brain barrier, there will be a delay in the time it takes for the brain to transform the medication to dopamine and, therefore, decrease or delay the medication’s efficacy.
Protein interactions with levodopa have been found to cause all four types of OFF periods. To maximize your ON times, avoid protein when you take your levodopa and talk to your doctor about how dietary changes can help you get the most from your medications.
Fiber
Like water, fiber-rich foods help reduce OFF times by reducing constipation. Constipation slows the movement of food through your gastrointestinal tract, thereby slowing the process by which your levodopa is converted to dopamine. If your intestines aren’t being emptied regularly, the levodopa you take won’t pass through the digestive system as it should, and, therefore, you will feel OFF more often.
How can fiber help? Dietary fiber—non-digestible carbohydrates found in all plant foods, including fruits, vegetables, grains, nuts, and seeds—consists of insoluble and soluble fiber, which work together to make your stools larger, softer, and capable of passing smoothly through your bowels. Though it may seem counterintuitive, a bulkier stool is easier to pass than a smaller and watery one. Seeking out a wide variety of high-fiber foods will help you manage constipation and, in turn, minimize OFF times.
How exercise can reduce OFF times
Exercise, just like water and fiber, can help you feel more ON each day by helping to minimize constipation. Different forms of exercise help in different ways. Aerobic exercise increases your heart rate and gets your blood pumping quickly, stimulating the intestinal muscles. This can help the muscles contract, which in turn helps move stools more quickly. Yoga can help manage constipation as well; certain poses, such as downward-facing dog and cat-cow, increase blood flow to the digestive tract and, like aerobic exercise, help stimulate intestinal contractions.
 In addition, exercise can help you feel ON more often by managing your symptoms themselves. Research and anecdotal evidence continue to highlight the critical importance of exercise for people with Parkinson’s, showing how it can improve mobility and coordination, boost your mood, reduce stiffness, and minimize soreness and fatigue. (And each year, more studies prove that exercise may slow the progression of Parkinson’s itself, meaning it can help you feel more ON for more years.)
In addition, exercise can help you feel ON more often by managing your symptoms themselves. Research and anecdotal evidence continue to highlight the critical importance of exercise for people with Parkinson’s, showing how it can improve mobility and coordination, boost your mood, reduce stiffness, and minimize soreness and fatigue. (And each year, more studies prove that exercise may slow the progression of Parkinson’s itself, meaning it can help you feel more ON for more years.)
In addition to possibly slowing the progression of Parkinson’s, aerobic exercise can help minimize OFF times right away. It helps reduce motor symptoms such as rigidity, stiffness, slowness, and postural instability, and it has also been shown to reduce tremors in people with Parkinson’s. It can positively impact gait, balance, and functional mobility, as well as fine motor skills. As importantly, exercise has been shown to reduce non-motor symptoms of Parkinson’s, including sleep problems, constipation, digestion, depression, fatigue, and cognitive decline. In short, regular exercise helps you feel ON more often.
How continuous dopaminergic stimulation can help prevent or minimize OFF times
As Parkinson’s progresses, your brain produces less and less dopamine. This means it must rely much more heavily on levodopa to control your symptoms. Yet as Parkinson’s progresses, many people begin to experience fewer benefits from their medications, and the benefits may also be less consistent. This can increase your wearing OFF periods and ON-OFF fluctuations.
Several years ago, Parkinson’s researchers found that once dopamine terminals have degenerated a certain amount, intermittent doses of levodopa lead to “dramatic peak and trough fluctuations,” which ultimately results in the development of motor complications. They developed the hypothesis that continuous delivery of levodopa—a concept known as continuous dopamine stimulation (CDS)—might be associated with a reduced risk of these motor complications.
The goal of CDS is to help the brain maintain more constant levels of dopamine; it does this by imitating the brain’s normal continuous pattern of stimulating dopamine receptors. By keeping dopamine levels more constant over 24 hours, CDS can help reduce OFF times, improve sleep quality, and positively impact quality of life.
Subcutaneous apomorphine infusion
One CDS treatment option is subcutaneous apomorphine infusion. During this procedure, apomorphine is administered through a portable, battery-powered mini-pump that injects the medication under your skin, usually into your abdomen. Open-label studies have long shown that apomorphine infusion effectively reduces OFF times, and results from a 2018 randomized, placebo-controlled, double-blind, multicenter trial showed that apomorphine infusion resulted in a clinically meaningful reduction in OFF periods for people with Parkinson’s who experienced persistent motor fluctuations.
Carbidopa/levodopa enteral suspension
Another CDS therapy is continuous carbidopa/levodopa enteral suspension, a Parkinson’s medication delivery system for people experiencing persistent ON/OFF fluctuations, especially those with advanced Parkinson’s. In this treatment, a carbidopa/levodopa gel suspension is delivered through a surgically implanted tube directly into the small intestine, where the medication is absorbed. This medication delivery directly into the small intestine has the added benefit of bypassing the stomach, the emptying of which can become unpredictable or delayed for people with Parkinson’s. The small pump, which you carry or wear, allows infusion of a constant medication dose over 16 hours each day, with your physician’s ability to prescribe additional doses at certain times. Research shows that carbidopa/levodopa enteral suspension improves ON/OFF fluctuations, activities of daily living, and health-related quality of life during short-term (12-week) treatment. Just as importantly, its positive impacts on motor fluctuations were largely sustained over the longer term, up to seven years.
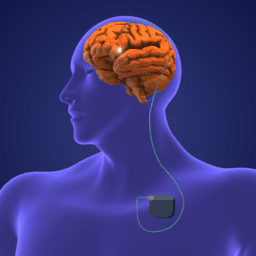
Deep brain stimulation
Deep brain stimulation (DBS) is another form of continuous stimulation that can significantly reduce OFF times. DBS is a neurosurgical procedure in which electrodes are implanted into specific regions of the brain. These electrodes emit continuous electrical impulses (stimulation) from a stimulator device, similar to a cardiac pacemaker implanted in the chest. While DBS does not affect dopamine levels in the brain (instead, it compensates for the secondary effects of dopamine loss), often this treatment leads to more ON times and improvements in many Parkinson’s motor symptoms such as tremor, stiffness, and slowness.
Extended-release medications
Although not a “continuous” therapy, extended-release medications can help reduce OFF times by providing a more constant level of levodopa in the bloodstream and the brain. In clinical studies, the extended-release carbidopa/levodopa drug Rytary® demonstrated a two-times reduction in OFF time during waking hours. Other treatment options that can minimize OFF times through extended delivery include the rotigotine patch, extended-release pramipexole, and extended-release ropinerole.
Take Action
As you can see, numerous strategies can help you limit (and for some, eliminate) your OFF times, maximize your ON times, and live your best life with Parkinson’s. Don’t assume that OFF is a Parkinson’s “given”—take action TODAY so you can live well now and for years to come.
This post was written by the Davis Phinney Foundation.
This blog series is sponsored by Amneal.
Thank you to our 2021 Peak Partners