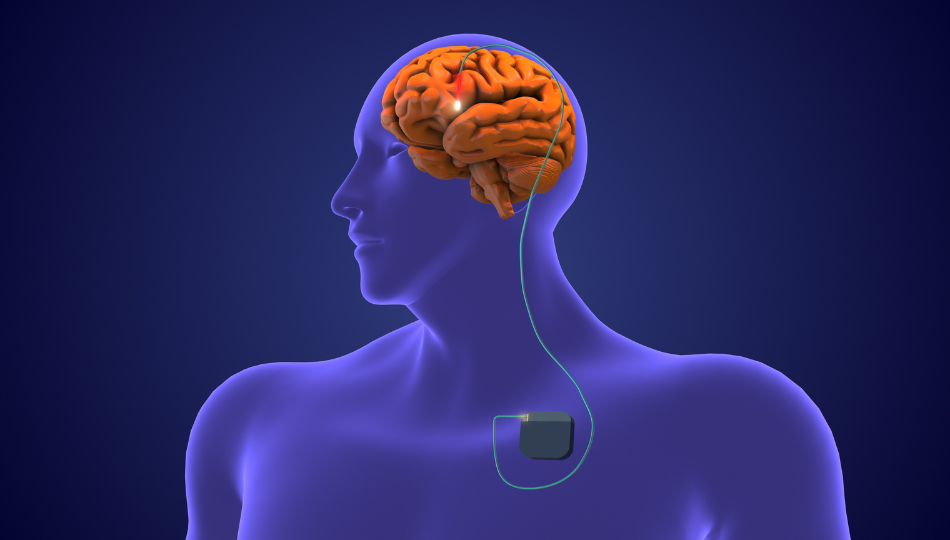
Making the decision to have Deep Brain Stimulation (DBS) is complex. On one hand, by the time you’re considering it, your Parkinson’s symptoms have likely become difficult to manage with medications, and you’re probably experiencing motor fluctuations. On the other hand, there are many things to consider–and feel–about the idea of having brain surgery. Because the decision to have DBS surgery is a big one, we often receive questions about what you can expect in the days, weeks, and months immediately after DBS surgery. Here, we address some of the topics we’re frequently asked about the DBS recovery timeline.
Getting started with DBS involves multiple steps, and the full process almost always involves several surgical procedures. It’s also important to know that although surgical complications can occur, DBS surgery is widely considered to be a safe procedure. Rates of complication are low and most people return home after surgery within a day or two.
Read on for seven other things to know about recovery from DBS surgery.
RECOVERY IS A MULTI-STEP PROCESS: TAKE IT SLOW
You should leave the hospital with detailed instructions about what to do—and what not to do—in the days and weeks following your final DBS surgery, but here are some central things to keep in mind:
- You are likely to be able to perform most of your usual activities of daily living within a few days of your surgery. In fact, after surgery, you won’t leave the hospital until you demonstrate your ability to perform basic tasks: sitting, standing, walking, and using the bathroom. Most people resume the bulk of their normal activities within a month, excluding strenuous exercise.
- You will have incisions that require care and may be uncomfortable. Post-operative pain is usually mild, but you will likely be prescribed an oral pain medication to take as needed. Follow your surgeon’s advice regarding its use. Most surgeons recommend people switch from prescription pain relievers to acetaminophen as soon as possible. Please follow your own care team’s recommendations or over-the-counter medication.
- While post-surgical complications like infection are uncommon, reduce your risk by lessening your activity level and taking it easy for as long as is recommended by your surgeon and care team. It is commonly advised to take time off of work, avoid strenuous activity for the first two weeks, and avoid lifting more than 20 pounds for the first four to six weeks after surgery. Each person’s activity limits vary.
- After surgery to place your DBS lead(s), you may experience a “honeymoon effect,” during which your symptoms improve even though your DBS system is not yet functional. This is likely due to microlesions that occur during surgery, and the effect will be temporary. Don’t modify your medication regimen during this time unless advised to do so by your care team.
- Your care team may advise you not to drive or fly for two weeks after your last surgery.
- Plan to have someone with you at home for the first few days of your recovery to help you and to monitor for signs of confusion or other complications requiring advice from your surgeon or emergency care.
Because your individual circumstances are likely to involve distinct recovery advice from your care team, be sure to leave the hospital with a hard copy of all recovery instructions and restrictions. Consider this example of post-operative instructions you may receive.
PRE-SURGICAL CHOICES CAN INFLUENCE YOUR RECOVERY
Decisions made before your surgery influence your recovery timeline.
Some of these decisions will essentially be surgeon or surgical center preferences. The most important considerations are that the surgeon has experience with the procedure they will perform and that you have rapport with them. Trusting your surgical team is important: You want to know they will be responsive to your concerns and that you understand what they say–especially in case you experience any post-surgical complications.
Choices that can influence your recovery timeline include:
The number of leads you have placed
If you are having bilateral leads placed, your surgeon may prefer to place them both at the same time or to place them during separate surgeries. It may sound tempting to minimize the number of surgeries and have multiple leads placed at once, but this extends the duration of the surgery, which can contribute to higher surgical risks.
On the other hand, being under anesthesia can affect your symptoms and medication regimen, and you may prefer to minimize the number of times you experience anesthesia to minimize these complications. Discuss these considerations with your care team before scheduling surgery.
The TYPE OF ANESTHESIA you receive
Although the risk profiles between DBS surgery under general anesthesia (you’re unconscious during a procedure) and local anesthesia (you’re conscious and the area of your body undergoing surgery is numbed) are similar, some studies have found fewer adverse events following DBS surgery under general anesthesia.
In 2023, Guo and Gao published results of a clinical trial comparing outcomes of 66 people who underwent DBS surgery with general anesthesia and 66 people who underwent the procedure using local anesthesia. The general anesthesia group experienced lower rates of post-operative headache, dizziness, vomiting, and delirium.
Guo and Gao also observed that the general anesthesia group had lower levels of stress regarding their surgery and that the surgeries under general anesthesia were an average of an hour shorter. Moreover, people who had general anesthesia were able to walk and check-out of the hospital sooner than those who had DBS surgery under local anesthesia.
Perhaps the most important consideration on this subject is that DBS under general anesthesia may be better for you if you experience restlessness, anxiety, or dystonia during OFF periods. While there are ways to manage these symptoms during DBS surgery under local anesthesia, you might prefer to have the surgery under general anesthesia if you are likely to experience them.
Where your battery/PULSE GENERATOR is placed
Whether your battery/pulse generator is placed directly under your skin or whether it is placed under your muscle may also influence your recovery. Generally, surgeons place the device under the muscle if a person is particularly thin. There is limited data about recovery differences between these options, but you may have more soreness and range of motion limitations if your battery is placed under your muscle. These effects are temporary.
POST-SURGICAL COMPLICATIONS OCCUR, BUT ARE INFREQUENT
In 2023, researchers from the Barrow Neurological Institute and Muhammed Ali Movement Disorders Clinic, Olson et al., wrote a systematic review of risks associated with DBS surgery for Parkinson’s. The authors reviewed 34 articles as part of their research, and summarize their results by saying that when candidates for DBS are carefully screened, DBS is a relatively low-risk procedure.
Important details from Olson et al.’s research include:
- Common post-operative complications include infection, hemorrhage, confusion, and delirium.
- Over 20,000 people were included in the reviewed studies presenting data about deaths associated with DBS surgery. Mortality rates were less than 0.5%. According to a 2014 systematic review, this is comparable to the 30 to 90 day mortality rate following hip replacement surgery.
- A 2014 study involving 1,757 people who had DBS surgery found 7.5% of people had a post-operative complication within 90 days of having DBS surgery. The most common complication was wound infection (3.6%), followed by pneumonia (2.3%), hemorrhage (1.4%), and pulmonary embolism (0.6%).
- A study involving over 32,000 people who had DBS surgery found that 4.4% of people experienced a post-surgical complication. The most common complication, urinary or kidney issues–typically a urinary tract infection–occurred in less than 2% of people. This type of post-surgical complication can occur after any surgery. For example, it is 50% more common following joint replacement surgery than it is following DBS surgery.
- Some complications may result in additional hospitalization or a longer post-operative stay in the days after surgery. These include bleeding, inflammation, infection, reactions to anesthesia, and DBS hardware malfunction.
- In studies of up to 6,058 people who had DBS surgery, all but one study reported hospital readmission rates following DBS surgery of under 5%. The one study with a higher rate of readmission (15%) included those who were readmitted to address some aspect of their DBS hardware.
- Risk factors associated with increased rates of post-operative complications include: older age at time of surgery, lower pre-operative cognitive ability, greater deficits in attention and visuospatial processing, obesity, and cardiovascular comorbidities.
In their 2022 study of 426 people who had DBS surgery, Jung et al. corroborate many of Olson et al.’s findings.
PROGRAMMING WILL TAKE TIME
In a 2022 article about DBS programming, Shukla et al. write, “successful DBS programming is usually accomplished over a period of three to six months. Programming is usually not initiated immediately after the placement of a lead; instead, a time frame of 2–4 weeks is allowed for the microlesion effects to fade away.”
Other things to know about programming:
- You will likely be asked to attend programming visits–especially early ones–after having skipped one or more doses of your medication. If this will be intolerable to you, or you don’t have a care partner at home to help, you may be able to have your programming performed as an in-patient procedure.
- Your initial programming visit may last over an hour.
- It is common for the effectiveness of your programming parameters to change over a period of days or weeks.
- It may take six or more programming sessions before your programming is optimized. It is very rare for optimal programming to be established in fewer than three sessions. DBS doesn’t affect progression of Parkinson’s, so you will also have regular visits to continue to modify your system’s programming after your initial optimization.
- You may experience dyskinesia immediately after your programming starts or hours or even days after your first visit. Don’t be discouraged: This often means your DBS leads are well-positioned, and it can be managed by reducing medication or stimulation parameters.
- Don’t be alarmed if your speech is affected during your DBS programming process. Slurring of speech happens, but is typically mitigated by changing programming parameters.
- You may be given the ability to modify your programming on your own within pre-determined limits. If you have questions about this process before you leave the clinic, be sure to ask them and have the answers put in writing for you. Keep a notebook at home to jot down questions that occur between programming visits.
YOUR SYMPTOMS MAY CHANGE AND FLUCTUATE
In addition to the possibility of fluctuating dyskinesia after DBS programming, other symptoms may change during the initial weeks and months after surgery. For example, França et al. write that pain, sleep, and behavioral fluctuations may improve. These improvements may be affected by medication adjustments required to optimize your programming.
Additionally, Shukla et al. observe that programming efforts to suppress dyskinesias may worsen bradykinesia, especially when DBS leads target the globus pallidum.
DBS does not improve motor symptoms that aren’t improved with dopaminergic treatment. You should have a discussion about this during your pre-operative assessments with your care team. If it is not made clear, be sure to ask which of your symptoms your team expects to improve most and which symptoms they expect to improve least. This will help ensure you are having the procedure with a strong and reasonable understanding of what to expect.
YOU MAY GAIN WEIGHT
Weight gain after DBS surgery is not uncommon. In a 2019 analysis of research about DBS and weight gain, Steinhardt et al. found that by 12 months following DBS surgery, people with Parkinson’s gained an average of 14 pounds.
The exact reasons for this are not well understood, but multiple factors appear to be involved. For example, some research suggests sense of smell and taste can be improved by DBS and increased dexterity may help you eat more. A more well-established theory is that DBS improves rigidit, rest tremor, and dyskinesia, which results in lower energy expenditure.
YOUR ACTIVITIES MAY need TO CHANGE
While your initial recovery will take a matter of weeks, your DBS system requires a few important longer-term limitations.
For example, there are case studies of swimming ability being impacted by DBS systems. DBS systems will not function properly if you scuba dive below 33 feet. Be careful when swimming and confirm your ability to swim in a controlled environment before you go diving.
There are other things you should avoid after DBS surgery. These include:
- Anything that might subject your head and neck to unnatural torque, like skydiving or some amusement park rides
- Prolonged exposure to temperatures above 100 degrees Fahrenheit as in a sauna, hot tub, or tanning bed
- Transcranial magnetic stimulation
- Working with high voltage transmitters, arc welding equipment, and other high-powered electrical equipment; standard in home microwaves and electric appliances are not cause for concern
- Recreational activities in which you are unable to protect the pulse generator from impacts.
You should also tell any surgeons or imaging technicians, as well as any airport screening personnel, about your DBS system. The wands used by airport safety screeners may cause errors if they are held too closely to the pulse generator for too long. Also, plan to include your patient controller in carry-on baggage when traveling by air, in case you need it.
Advancing Technology and recommendations
DBS technology is advancing, and the number of experienced surgeons and surgical centers is growing. Moreover, researchers continue expanding our understanding of best practices for DBS surgeries, including outcomes for people in earlier stages of Parkinson’s who receive DBS.
DBS can dramatically improve symptoms and quality of life for people living with Parkinson’s. The surgical process is not without risk, but for many people who have had DBS surgery, the risks are outweighed by the outcome. In fact, a 2019 study found of 320 people who had DBS surgery, 95% would recommend DBS to others.
Every person’s risk tolerance and interest in DBS is unique, but with careful attention to recovery guidance—and a bit of patience with the programming process—most people who have DBS surgery experience substantial benefit and few surgical complications.
ADDITIONAL RESOURCES
DBS Resources from the Davis Phinney Foundation
Mechanisms and Consequences of Weight Gain after DBS
DBS Information Session Slides from University of California, Davis
DBS in Parkinson’s: Past, Present, and Future
Short-Term Motor Outcomes After DBS Combined with Post-Operative Rehabilitation
General Anesthesia vs Local Anesthesia in Microelectrode Recording-Guided DBS
STN and GPI DBS for Parkinson’s—Meta-Analysis of Outcomes
This DBS educational content is supported by a grant from Medtronic. This content was independently written by the Davis Phinney Foundation.