“When I was OFF, I’d have tremors in my hands, and sometimes also in my legs and feet, and I would be slower in my movements across the board. My arms wouldn’t swing when I walked, and I’d shuffle my feet. Depression, apathy, and anxiety was often present for me, too.”
Doug Reid, a Davis Phinney Foundation Ambassador living with Parkinson’s for 13 years
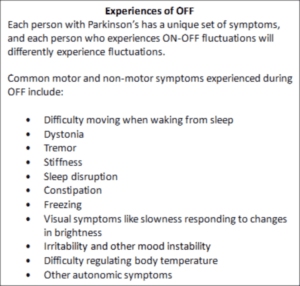
Experiences like Doug’s are common as Parkinson’s progresses, which is challenging not only for those living with the condition but also their family and care partners. This experience is common: As Parkinson’s progresses, the neural circuitry in the brain becomes damaged, and the effects of Parkinson’s medications begin to fluctuate—sometimes unpredictably. When medications are working well, a person is described as being ON, and when the medications are working less well—as in Doug’s case—a person is described as being OFF.
Dr. Cherian Karunapuzha from the Meinders Center for Movement Disorders in Oklahoma City compares these damaged neural circuits to a switch box that codes for our movements. When the thinking part of the brain decides to do something—like reaching for a coffee mug—the planning part of the brain relays the information to the switch box. The switch box then does two things:
- It switches on all the relevant programs needed to kickstart the activity.
- It switches off all the unwanted things that should not be happening while you reach for the mug.
In a brain unaffected by Parkinson’s with the switch box working well, reaching for the coffee mug is a seamless, smooth movement. The brain switches all the relevant programs on and off, relaying information back to the spinal cord, nerves, and muscles, resulting in movement.
The unique thing about the circuit described above is that the nerves operating within the circuit use a chemical called dopamine to communicate. For people living with Parkinson’s, the nerve cells that process and produce dopamine become impaired.
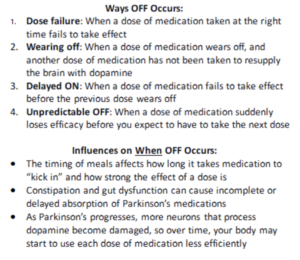
In the early stages of Parkinson’s, the effect of treatment is often smooth. Unfortunately, as Parkinson’s progresses, nerves become more and more damaged and are less able to recycle dopamine. This is when people start to experience ON-OFF fluctuations: As the brain becomes less capable of using dopamine, medications become less effective, leading to inconsistent symptom management. Thus, as Parkinson’s progresses, you may need to increase your treatment frequency to manage symptoms, and the window of relief from each dose of medication becomes shorter.
As with everything related to Parkinson’s, there’s no clear, predictable, or linear path. Sometimes, even from day to day and moment to moment, ON-OFF fluctuations can be erratic—as if someone is flipping a switch on and off. Other times, it can be as if a light switch is caught halfway between on and off, and the light buzzes and flickers.
Ways to Manage OFF Times
#1 – Talk About OFF with Your Care Partners and Medical Team
To best manage ON and OFF times, you must be open and honest with your care team. Because OFF times can unpredictably occur, it’s important to candidly talk with care partners about your experience of OFF and their experience of your OFF times, including what they might notice happening before, during, and after an OFF period.
You can develop various strategies to help navigate OFF times. Consider leaving notes on doors to remind you and your care partner to bring doses of your medication when you go out, adjusting your meal schedule to accommodate your medication schedule, and setting regular alarms to remind yourself to drink adequate water.
In preparation for future appointments, it’s helpful to keep a journal to document when you take medications, when you experience OFF times, and what symptoms are involved in your experience. Having a care partner or friend join you for appointments is beneficial, too.
#2 – Work with Physical and Occupational Therapists
Physical therapists help manage OFF periods by helping you strengthen muscles, improve balance, and develop strategies to respond to problematic symptoms—including gait issues.
Occupational therapists help develop strategies to improve your ability to safely navigate aspects of your daily life at work, in public, and at home, which all may be complicated by your experiences of OFF times.
#3 – Eat Well, Exercise, and Stay Hydrated
Diet and exercise are among the most essential tools for navigating OFF. Your diet can influence OFF times by contributing to constipation and poor medication absorption, so talk to your care team about whether you should modify your diet.
Hydration is a related factor in managing OFF. Adequate hydration helps manage ON-OFF fluctuations by positively affecting constipation, medication absorption, and other Parkinson’s symptoms like orthostatic hypotension.
Exercise influences metabolism, which is known to help with constipation and medication absorption. Exercise has broad positive effects on Parkinson’s symptoms like rigidity and slowness; research indicates that exercise may even be able to slow Parkinson’s progression.
#4 – Consider Adjunct and Advanced Treatments
Treatments for Parkinson’s disease aiming to decrease OFF time include extended/controlled-release formulations of dopamine therapies to extend how long each dose lasts, fast-acting treatments to quickly supply dopamine to help you return to an ON state, and advanced therapies which aim to supply a continuous supply of dopamine by bypassing the digestive system.
Other new therapies—including continuous subcutaneous supply of dopamine—are being researched in clinical trials and reviewed by the FDA.
Additional Resources
Interactive Infographic: The Brain as a Switchboard
OFF: What It Is and How to Manage It
Managing Motor Symptoms During OFF
Parkinson’s 101, including discussion of ON and OFF
Why You Must Drink Water with Your Parkinson’s Medications
References
- https://www.uptodate.com/contents/medical-management-of-motor-fluctuations-and-dyskinesia-in-parkinson-disease
- https://www.uptodate.com/contents/medical-management-of-motor-fluctuations-and-dyskinesia-in-parkinson-disease
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Parkinsons-Disease#:~:text=Parkinson’s%20disease%20is%20a%20progressive,an%20important%20chemical%20called%20dopamine.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5685546/
- https://www.neurologylive.com/view/maximizing-on-time-longer-lasting-levodopa-therapy-options-for-parkinson-s-disease
- https://www.nature.com/articles/s41531-023-00541-w
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9046970/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8095707/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5856226/
- https://www.sciencedirect.com/science/article/abs/pii/S0074774219300236
- https://pubmed.ncbi.nlm.nih.gov/21311363/
- https://www.health.harvard.edu/diseases-and-conditions/common-causes-of-constipation
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5685546
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5856226/
- https://pubmed.ncbi.nlm.nih.gov/21311363/
This post was written by the Davis Phinney Foundation.
This post is sponsored by AbbVie Inc.