Impulse-control and related disorders (ICBDs) are challenging in many ways: They can drain bank accounts, destroy relationships, and have many other devastating effects. Examples of ICBDs include pathological gambling, compulsive sexual behavior, binge eating, compulsive shopping, compulsive hobbyism, punding, and dopamine dysregulation syndrome (DDS).
ICBDs aren’t rare. Baig et al. shared that up to 20% of people living with Parkinson’s experience ICBDs, while up to one-third of people living with Parkinson’s experience some degree of ICBD, even if they do not meet the formal criteria for diagnosis of ICBD. Among people who take dopamine agonists, incidence of ICBDs is even higher: Corvol et al. Found that up to 52% of people who took a dopamine agonist over a five-year period experienced an ICBD.
Although there are limited high-quality studies of treatment efficacy for ICBDs, in January 2024, a team of experts organized by the Movement Disorder Society published a consensus statement about how to manage these disorders. This statement involved a survey of 53 experts, of whom almost all had more than 10 years’ experience treating people with Parkinson’s experiencing an ICBD.
IDENTIFYING AND DEFINING SEVERITY OF IMPULSE-CONTROL DISORDERS
Managing ICBDs starts with recognition. We’ve discussed this subject in a blog post published in 2018, and the new consensus statement, written by Ines Debove and a team of 30 other experts, highlights three common features of ICBDs:
- Impulsivity: When a person fails to resist a temptation to perform a behavior
- Compulsivity: When a person repeatedly demonstrates lack of self-control over a behavior
- Functional Impact: When there are negative consequences of the impulsive or compulsive behavior
Debove et al. note that impulse control disorders may benignly begin, perhaps with a non-problematic increased interest in an activity. Because apathy can be a challenge for people with Parkinson’s, this increased interest may be viewed as a positive development. However, over weeks, months, or years, the behavior may become problematic.
Since ICBDs exist on a spectrum from non-problematic to immediately dangerous, Debove et al. propose grading the severity of ICBDs from 0-4.
PUNDING AND DOPAMINE DYSREGULATION SYNDROME
Punding and DDS are two unique ICBDs. Compared with other ICBDs, they are more frequently seen in people who take high doses of levodopa. While there is limited research about this, Debove et al. note this suggests punding and DDS may have a distinct biological cause and that the best treatment strategies will differ, as well.
MANAGEMENT OF IMPULSE CONTROL DISORDERS
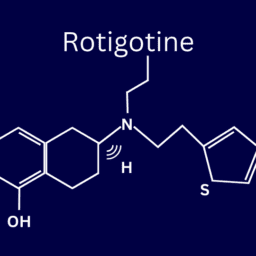
Debove et al. share that there is extremely limited high-quality research about optimal treatment for ICBDs. Existing research and experience of clinicians, however, suggests that the core management strategy is to decrease the dose of dopaminergic medications taken by someone experiencing ICBDs. Because dopamine agonists are significantly associated with ICBDs, the most common management strategy used by specialists consulted in production of Debove et al.’s consensus statement was to decrease dopamine agonist doses. 92% of the specialists surveyed used this strategy.
Decreasing doses of dopamine therapy is likely to have other effects on your Parkinson’s symptoms, so it’s important to involve your care team in managing any changes to your medication regimen.
DOPAMINE AGONIST WITHDRAWAL SYNDROME
The risk of dopamine agonist withdrawal syndrome (DAWS) is a critical reason to involve your care team in adjustments to your medications.
Debove et. al. define DAWS as significant worsening of one or more nonmotor symptom of Parkinson’s following discontinuation or tapering of a dopamine agonist. Symptoms of DAWS include anxiety, panic attacks, depression, agitation, irritability, drug craving, insomnia, daytime fatigue, nausea, vomiting, flushing, and generalized pain. New or worsened apathy is a possible long-term effect of DAWS.
OTHER RECOMMENDATIONS IN THE CONSENSUS STATEMENT
In addition to decreasing dopaminergic therapy dosage, other strategies recommended by the specialists involved in developing the consensus statement include:
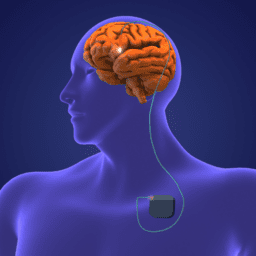
- Bilateral deep brain stimulation (DBS) of the subthalamic nucleus, recommended by 73% of specialists
- Cognitive behavioral therapy (CBT), recommended by 73% of specialists
- Reversal of last medication change prior to onset of ICBD, recommended by 69% of specialists
- Quetiapine and clozapine, recommended by 69% of specialists
- Selective serotonin reuptake inhibitors (SSRIs), recommended by 62% of specialists
COMMON STRATEGIES: PROS AND CONS
Debove et al.’s consensus statement also includes discussion of some nuances to the use of the strategies mentioned above.
DEEP BRAIN STIMULATION
Multiple studies have found reductions in ICBDs after bilateral DBS of the subthalamic nucleus. The efficacy of DBS is less clear when stimulation is unilaterally applied to the subthalamic nucleus and globus pallidus internus.
COGNITIVE BEHAVIORAL THERAPY (CBT)
There has been evidence that CBT adapted to ICBDs is helpful, but the evidence is limited to small studies. CBT has not been shown to be helpful in managing DAWS.
INVOLVEMENT OF SIGNIFICANT OTHERS
Involvement of significant others can help improve outcomes for people experiencing DDS, but there’s limited evidence for more aggressive care partner interventions like blocking credit cards or having the care partner manage distribution of medications.
SHORT-ACTING VERSUS LONG-ACTING FORMULATIONS
In addition to lowering doses of dopaminergic therapy, using short-acting formulations of medications rather than long-acting or extended-release formulations has shown as less likely to cause ICBDs.
CONTINUOUS LEVODOPA
Two studies showed that continuous levodopa infusion via the Duopa™ system correlated with improvements to ICBDs. Debove et al. speculate that the cause of this is the regularity of the therapy which leads to stable levels of levodopa in the body rather than fluctuations that occur with oral medication. Fluctuations might lead to greater likelihood of seeking excess dopamine from compulsive or impulsive behavior.
ADJUNCTIVE MEDICATIONS
Although one clinical trial showed that amantadine improved ICBDs, multiple other studies showed that it was correlated with onset and worsening of ICBDs.
Clozapine and quetiapine, drugs for schizophrenia and depression, have shown in small studies to be helpful for managing ICBDs.
Additionally, there is research suggesting that selective serotonin reuptake inhibitors (SSRIs) can help compulsive gamblers decrease their gambling behavior, but this research did not involve people with Parkinson’s. Moreover, there is also some evidence that, in general, ICBDs are more common in people who take these medications.
SPECIFIC STRATEGIES FOR PUNDING AND DOPAMINE DYSREGULATION SYNDROME
An engaged care partner, clozapine, continuous levodopa, and subthalamic DBS have been shown to be effective for DDS in a small study. Taking smaller but more frequent doses of levodopa might help, too.
There is limited research into treatments for punding, but one study found a multistep approach that helped. The approach included:
- Avoiding levodopa before bed
- Avoiding rescue formulations of levodopa
- Reduction of levodopa and/or dopamine agonist dosage
- Use of a COMT inhibitor or alternative dopamine agonists in event of worsening motor symptoms
- Amantadine, quetiapine, or clozapine as needed to manage symptoms
MORE RESEARCH NEEDED
The consensus statement from the Debove et al. is helpful and informative, but one of the central takeaways is that more research into ICBDs is needed.
Existing studies on this subject are simply too limited to establish rigorous certainty about best practices for managing ICBDS. Despite this limitation, the collection of clinical expertise presented by Debove et al. offers compelling advice to help you and your care team navigate one of the most difficult and dangerous aspects of living with Parkinson’s.
It is possible for you and your care team to manage and resolve ICBDs. We are here to help. If you have questions, please email us at blog@dpf.org.
ADDITIONAL RESOURCES
Family Dynamics of Parkinson’s
Impulse Control Disorders Blog Posts
Impulse Control Disorders in Parkinson’s
Long-Term Follow-up of Impulse Control Disorders in Parkinson’s
 WANT MORE PRACTICAL ARTICLES LIKE THIS?
WANT MORE PRACTICAL ARTICLES LIKE THIS?
You can learn much more about living well with Parkinson’s today through our Every Victory Counts® suite of resources. Each manual is packed with up-to-date information about everything Parkinson’s. Click the link below to reserve your manual(s).
Thank you to our 2024 Gold Partner, AbbVie, and our Silver Partner, Mitsubishi Tanabe Pharma America, for their ongoing support of these must-have manuals. Additionally, we’d like to thank Barbara and Dale Ankenman, Abby and Ken Dawkins, Bonnie Gibbons, Irwin Narter, Lorraine and J Wilson, and Gail Gitin in loving memory of Gene Gitin for their generous donations that allow us to make these resources available and accessible to all.