Many people who are in the early stages of thinking about or planning for deep brain stimulation (DBS) don’t realize there are therapy consultants they can talk to about the process, the device, and how it all works. So, we were grateful to have the chance to talk to Alaine Keebaugh, PhD, and potential DBS recipient Scott Rider about the value of building a relationship with a therapy consultant, using a Boston Scientific DBS system.
Topics discussed include:
- Parkinson’s medicine
- Role of therapy consultant
- How does a Boston Scientific DBS therapy consultant become involved?
- How did you meet your Boston Scientific DBS therapy consultant?
- Different companies offering DBS
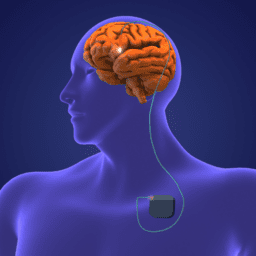
- About the rechargeable devices
- What are your concerns as a patient?
- What is the longevity of the device?
- What symptoms may be reduced with a Boston Scientific DBS?
If you want to learn what a therapy consultant can help you with as you navigate the DBS journey, watch, listen, or read below.
You can download an audio file of this webinar here: Audio Boston Scientific Therapy Consultant and Person with Parkinson’s .
You can download a transcript of this webinar here: Transcript Boston Scientific Therapy Consultant and Person with Parkinson’s .
You can also read it below.
Note: This is not a flawless, word-for-word transcript, but it’s close.
*While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.