You’ve taken the time to process your Parkinson’s diagnosis. You’ve started exploring trusted resources about symptoms, treatments, and actions you can take to live well. You’ve embraced your feelings, grounded yourself, planned your course of action. You’ve experienced what Parkinson’s is like for you. How, though, do you communicate what Parkinson’s is (for you) to others?
Describing Parkinson’s to people who don’t have it is complicated for a number of reasons. To begin with, it is an exceptionally complex neurological disorder, and there are still numerous aspects of Parkinson’s that remain a mystery. Second, everyone’s experience with Parkinson’s is different. So, even if someone knows another person with Parkinson’s, what Parkinson’s is for you may be very different than what Parkinson’s is that other person. Third, you may be at the point where you’re not experiencing many symptoms, or the symptoms you are experiencing aren’t noticeable to others. And fourth, because Parkinson’s is simply a part of your life, not your whole life, you probably don’t want it to dominate every conversation!
So, when a friend, colleague, extended family member, or even a healthcare professional who knows only the basics of Parkinson’s asks you to explain it, what do you say? If you don’t wish (or have the time or energy) to paint an in-depth portrait of your unique Parkinson’s, but you do wish educate others, simply stick to the basics. To help, here’s a list of short, to-the-point Parkinson’s “talking points” you can pull out when you need them.
What is Parkinson’s?
- Parkinson’s is a complex neurological disorder associated with a loss of dopamine-producing nerve cells deep inside the brain
- Dopamine is a neurotransmitter (a chemical substance) that helps regulate the body’s movement
- Less dopamine in the brain means less control over movement and less mobility in general
- Parkinson’s is the world’s fastest growing neurological brain disease, affecting 1.2 million people in the US and an estimated 10 million people worldwide
- Parkinson’s is officially classified as a movement disorder because it involves damage to the areas of the brain, nerves, and muscles that affect the speed, quality, fluency, and ease of movement
- Common motor symptoms are tremor, stiffness, slowness, and postural instability
- While the effects of Parkinson’s on movement are often the most visible symptoms, non-motor symptoms can sometimes have an even greater impact on quality of life
- Common non-motor symptoms include constipation, sleep problems and fatigue, depression and/or anxiety, pain, and cognitive changes
- Parkinson’s is both chronic and progressive, which means symptoms will change and get worse over time. In other words, my Parkinson’s will never get better, though I hope treatments can help mask it as much as possible
- The rate of progression varies from person to person
- Everyone with Parkinson’s experiences symptoms differently, and not everyone with Parkinson’s experiences the same symptoms
What treatment options exist?
- Many pharmacological treatments for Parkinson’s work to replace or enhance lost dopamine
- Treatment typically includes some combination of medication, exercise, rehabilitation strategies (like physical, occupational, and speech-language therapy), and complementary therapies (like mindfulness and meditation, acupuncture, and many more), and sometimes surgical therapies
- The gold-standard medication for Parkinson’s is levodopa, a central nervous system agent that helps minimize symptoms because it is converted to dopamine in the brain
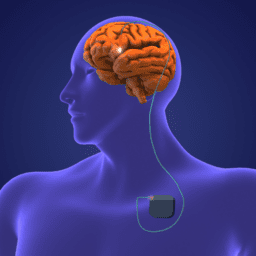
- Surgical therapies include Deep Brain Stimulation (DBS), carbidopa/levodopa enteral suspension (Duopa®), focused ultrasound, Transcranial Magnetic Stimulation, and more
What are some steps you can take to live well every day?
- Exercise regularly
- Address Parkinson’s through the whole picture of lifestyle, diet, exercise, stress management, relationships, and personal and spiritual care and growth
- Build a strong care team personalized to my unique needs and goals
- Connect with others
- Seek support from people who understand what I’m experiencing
- Explore creative outlets
- Give back
- Take it one day at a time
- Focus on the positive
Helping people understand Parkinson’s isn’t easy. Stereotypes, misunderstandings, healthcare, and the media have done a good job of either misrepresenting or stigmatizing people with Parkinson’s ever since it was first recognized as a disease. While it is not your job as a person with Parkinson’s to teach people about Parkinson’s (how exhausting!), finding people who are open, kind, and patient and sharing your story with them is a step toward creating a more inclusive environment for everyone living with it. Authentic conversations about Parkinson’s can create meaningful change. So, the next time you’re asked what Parkinson’s is all about, if you have the desire and energy, go ahead and teach them a little something.
Of course, your conversations about Parkinson’s will change over time and vary depending on the people you’re talking to. Share as much as you feel comfortable sharing. Find balance in your conversations. And remember that you know your Parkinson’s best, and you can guide conversations about it in the direction you choose.
More Resources on Communicating about Parkinson’s
How to Communicate What It Means to be OFF
How to Communicate with your Parkinson’s Doctors