After being diagnosed with Parkinson’s, one of the most common questions is “Why?” We have seen many exciting breakthroughs in recent research, but we still don’t have a clear answer as to exactly what causes Parkinson’s. However, there are several promising advances that suggest various roots of Parkinson’s, as well as new insights that challenge century-old assumptions.
DOPAMINE
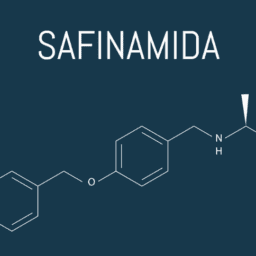
Brain cells called neurons communicate using specific chemicals called neurotransmitters. One type of neurotransmitter–dopamine–is produced by neurons in the brain, including in the substantia nigra (SN). Dopamine helps facilitate movement and is involved in reward-based behaviors and hormone release. There is an area of the SN called the substantia nigra pars compacta (SNpc) that is specifically comprised of these dopamine-producing neurons. When those neurons die, less dopamine is produced. A characteristic symptom of Parkinson’s is below-average levels of dopamine due to the death of dopaminergic neurons in the SNpc, which is why dopamine agonists are regularly prescribed for people with Parkinson’s.
When dopamine-producing neurons die and your body can no longer produce adequate levels of dopamine, motor control is impaired. Thus, the hallmark motor symptoms of Parkinson’s–tremors, bradykinesia, poor balance, involuntary movements–are clearly correlated with a lack of dopamine. However, motor symptoms usually do not begin to appear until there has already been about 60% dopamine neuron loss, and most people with Parkinson’s eventually lose 80% or more of their dopamine-producing neurons.
LEWY BODIES AND Αlpha-SYNUCLEIN
Another classic physiological marker of Parkinson’s is the presence of Lewy bodies: clumps of built-up protein found in certain neurons. In 2003, a researcher at Goethe University Frankfurt named Heiko Braak found that Lewy bodies show up in a predictable ordered pattern of brain regions. They often begin in the enteric nervous system, which controls gastrointestinal organs; the medulla, which is responsible for digestion, breath regulation, and heart function; and the olfactory bulb, which regulates smell. It makes sense, then, that losing the sense of smell and experiencing digestive issues (particularly constipation) are often the early symptoms of Parkinson’s. As Lewy bodies progress along the vagal nerve, different symptoms begin to present, eventually leading to motor symptoms as the Lewy bodies reach the SNcp.
Scientists have known for decades that Lewy bodies were made up in a large part by a protein called alpha-synuclein (α-synuclein). For many years it was assumed that they formed a jumbled clump of twisted fibers surrounding the Lewy bodies. However, researchers recently found that instead of the tangled mess of α-synuclein they were expecting, there was a variety of other organelles, including mitochondria and lipids. The α-synuclein was present, but not in the form they expected. While it has previously been suggested that α-synuclein buildup may cause Parkinson’s, this new research indicates that the buildup may instead be yet another symptom of an even deeper problem.
There is some overlap and confusion about the difference between Parkinson’s, Lewy body dementia (LBD), and Alzheimer’s. However, for people with Parkinson’s, Lewy bodies have been recorded since the early 1900s and are found within the SNpc as well as many other brain regions, including the amygdala, cortex, and locus coeruleus. Lewy bodies in these areas contribute to various Parkinson’s symptoms, including anxiety, depression, and cognitive difficulties.
LYSOSOMAL AND MITOCHONDRIAL DYSFUNCTION
As suggested above, emerging research suggests that rather than α-synuclein causing Parkinson’s, it may instead be representative of dysfunction of the mitochondria and lysosomes. Therefore, Parkinson’s may not be a protein problem as it is commonly described, but rather a cellular mechanistic problem instead.
The mitochondria are often described as the powerhouse of the cell since important biochemical processes–including cellular respiration and energy output–occur within them. However, when the mitochondria aren’t functioning correctly, they can begin to release reactive oxygen species (ROS) instead. Some ROS creation is normal, as they are formed as byproducts of oxygen metabolism and are used in processes like cell signaling. When something goes wrong, however, the overproduction of ROS can have serious negative effects.
Lysosomes, on the other hand, functions like the digestive and waste removal system in the cell. One of the waste products that lysosomes remove is α-synuclein. But when the mitochondria release ROS, the function of lysosomes can become damaged. If they can’t do their job and effectively remove cellular waste, α-synuclein begins to accumulate. As the protein builds up, characteristic Lewy bodies emerge and neurons begin to die off, producing Parkinson’s symptoms. This demonstrates a self-propagating loop in which a dysfunction within a single organelle like the mitochondria can cause a deleterious cascade into a downward spiral that eventually leads to Parkinson’s. Because these processes are normally so tightly regulated, one minor change can have serious effects down the line.
Further genetic research seems to support this hypothesis of a combined lysosomal and mitochondrial root of Parkinson’s. Researchers have found that some genes associated with Parkinson’s are also related to mutations that can cause lysosomal dysfunction. One study found that more than 50% of people with Parkinson’s have at least one allele (gene form) indicating damaged lysosomal function, and 21% have more than one. These findings suggested a link between the functionality of the lysosome and the presence of Parkinson’s. Further research confirms this idea because simulating lysosomal dysfunction has been shown to cause the buildup of α-synuclein and neuroinflammation, both characteristic of Parkinson’s.
Scientists are also looking into possible genetic and environmental causes of Parkinson’s. Several rare hereditary genes have been identified as markers of Parkinson’s in certain cases, and environmental effects like exposure to pesticides and herbicides, certain occupations, and drinking from contaminated wells have also been linked to Parkinson’s. However, there remain a great many cases that cannot be explained by those risk factors, so the search for explanations for Parkinson’s continues today.
WHAT CAN I DO TO BE PART OF THE ANSWER?
Research into these alternative explanations for Parkinson’s is ongoing. Clinical trials, including those testing medications currently used to treat lysosomal storage disorders, are already underway, and more are being added all the time. If you’re interested in being part of the answer to one of the most common Parkinson’s questions–“Why?”–check here for clinical trials near you. Nervous about signing up? Learn the 6 Myths of Parkinson’s Clinical Trials here.
GLOSSARY
- α-synuclein: A protein encoded by the SNCA gene that is produced largely in the brain. It is found at highly elevated levels in people with Parkinson’s and has been suggested as a cause for Parkinson’s. Its function is still largely unknown, but it may be involved in neurotransmitter release
- Allele: One form of a gene (of which there are at least two different forms) whose presence may result in a different phenotype
- Dopamine: A neurotransmitter that helps to facilitate movement, reward-based behavior, and hormone release. It is produced in the substantia nigra (SN) in the brain
- Lewy bodies: Clumps of proteins developed within neurons and found in high levels in people with Parkinson’s and people with Lewy body dementia. They are made of α-synuclein fibrils along with many other organelles, including mitochondria and lysosomes
- Lysosome: An organelle that acts as the digestive and waste removal system in a cell
- Mitochondrion: An organelle that conducts cellular respiration and outputs energy to the rest of the cell in the form of ATP
- Neuroinflammation: The brain’s immune system initiates inflammation of the nervous tissue in response to a stressor. Causes can be acute, like an injury or infection, but are more often chronic and in response to neurodegenerative diseases like Parkinson’s
- Neuron: A nerve cell that can communicate with other cells using electrochemical signals. Brain cells are referred to generally as neurons, though they also exist throughout the body
- Neurotransmitter: A chemical signal that allows neurons to communicate with each other. One example of a neurotransmitter is dopamine
- Reactive oxygen species (ROS): Chemically reactive chemical species containing oxygen
- Substania nigra pars compacta (SNcp): A subset of the substantia nigra. This part of the brain is made up of dopaminergic neurons and is primarily affected in people with Parkinson’s. Death of the dopamine-producing neurons in the SNcp correlates with the onset of motor symptoms
FURTHER RESOURCES
Is It Time to Rethink Parkinson’s Pathology?
Pathophysiology of Parkinson’s Disease
Braak Staging and Parkinson’s Brain Pathology
6 Myths about Parkinson’s Clinical Trials
WANT MORE PRACTICAL ARTICLES LIKE THIS?
Much more can be found in our Every Victory Counts® manual. It’s packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action. Request your free copy of the Every Victory Counts manual by clicking the button below.
Thank you to our 2020 Peak Partners, Amneal and Kyowa Kirin, with special support from Adamas for helping us make printing, distributing, and shipping the Every Victory Counts manual for free possible.