A few years ago, we were presented with an opportunity to collaborate with the Shirly Ryan AbilityLab to offer a one-year fellowship in Parkinson’s Disease (PD) and Movement Disorders (PDMD) Neurorehabilitation. We were thrilled when the very first PDMD Fellow, Ala Elyaman, DO, began in July 2021.
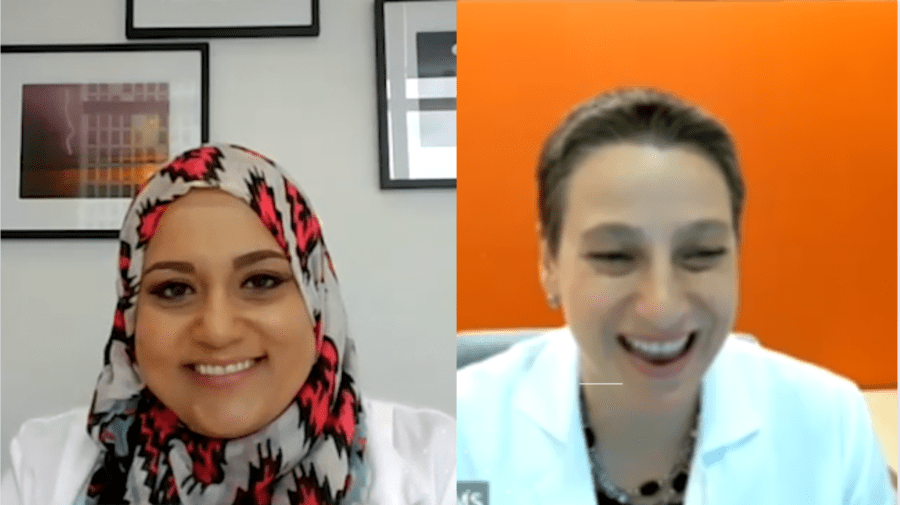
We had the chance to sit down with Dr. Elyaman and Dr. Jennifer Goldman, Shirley Ryan AbilityLab’s PDMD Section Chief, to talk about Dr. Elyaman’s first several months. You can watch the interview, read the transcript, or download the audio below.
An Interview with Shirley Ryan AbilityLab
You can read the transcript below or download it here.
Melani Dizon (Director of Education, Davis Phinney Foundation):
Hello everybody. My name is Melani Dizon. I’m the director of education for the Davis Phinney Foundation. And I’m really thrilled to be here today with Dr. Goldman and Dr. Elyaman, is that right? Elyaman. Elyaman.
Ala Elyaman, DO (PDMD Neurorehabilitation Fellow, Shirley Ryan AbilityLab): That’s perfect.
Melani Dizon:
And they’re both at Shirley Ryan AbilityLab. We have our very first fellowship that we have done. This was the brainchild of Dr. Goldman, I’m really excited to hear about sort of where this idea came from, and then what you Dr. Elyaman are doing right now and what you’ve been doing over the past six months since you started the fellowship. So, let’s dig in. Jennifer, can you tell us what is a PMDNR fellowship to begin with and how this idea come to be?
Jennifer Goldman, MD, MS (PDMD Section Chief and Movement Disorders Neurologist, Shirley Ryan AbilityLab):
Sure. Thank you so much Mel. We’re delighted to be able share information we have with you and the community today about this new fellowship and how excited we are about having a fellowship geared to Parkinson’s disease. And so, our Parkinson’s disease and movement disorder fellowship, which we’ve just abbreviated PDMD to alleviate a mouthful of topics. So, our Parkinson’s disease and movement disorders fellowship is a unique program. It’s a, one of the kind fellowship that is geared to training physiatrists or physical medicine and rehabilitation physicians in the principles of rehabilitation as they apply to Parkinson’s and movement disorders. And we know that the field of movement disorders is quite broad. We know Parkinson’s disease is one of the most common conditions that we see but we know movement disorders also includes other atypical Parkinsonian syndromes, tremors, gait disorders, Huntington’s, functional movement disorders, and other movement related conditions.
But there really hasn’t been at all in the field of psychiatry, specialized training in this area. And so, this is a very unique educational opportunity for fellows to learn about the field of Parkinson’s and movement disorders and gain clinical experience, mentorship, research experience, to be able to hone their skills and develop knowledge in this area. In recent years, there’s been a growing interest in the field of rehabilitation and how important it is in the care of people living with Parkinson’s. So, we typically think of rehabilitation as often, physical therapy, speech language pathology, and occupational therapy and perhaps also physical exercise and activities. But the role of the rehabilitation physician is an incredibly important role in the treatment and care plans for people living with Parkinson’s and their care partners. And we’ve started to see more and more studies and research in these areas that demonstrate how impactful rehabilitation can be on patient outcomes and also our awareness and our understanding of the scientific and evidence base behind them. And so, as a movement disorders neurologist who practices in interdisciplinary care settings in particularly Shirley Ryan AbilityLab as a rehabilitation hospital, this fellowship seemed like the ideal way to start addressing these gaps of knowledge in the field.
Melani Dizon:
Yeah, so interesting. So I would suspect that you know, people have been working and sort of collaborating on medical teams for forever, but when you have a movement disorder Fellow that has the physiatry, you, when you’re talking to the people who are working with people with Parkinson’s that are physical therapists, you guys are already talking the same language, like that’s all already there. And so, you have the ability to really go deep with that person. You are, you know, you have the science, the medical background, the research and then paired with that practical aspect of really helping that person get moving is pretty powerful. So, that’s very exciting. Dr. Elyaman what were you working on before you began this fellowship? And how did you find out about it?
Ala Elyaman:
I was in Miami doing my last year of residency in physical medicine and rehab or physiatry. And my program director ended up getting a flyer from Shirley Ryan AbilityLab talking about the program. And I was kind of at that point on the fence, do I wanna do fellowship, do I wanna do general rehab and, you know, just start working? And when I saw the flyer, it was, you know, like a light bulb went off. I was like, this is it. This is what I wanna do. It’s something new, it’s something, you know, exciting. I’ll get to learn a lot and get a lot of that one-on-one time with patients and also learn more about a field of rehab that even though it should be a big part of what we do, usually when we see Parkinson’s patients, it’s in the inpatient, you know, setting as a physiatrist, I mean, but it’s in the inpatient setting and it’s when they’ve had some other type of, you know, misfortune like a fall or, you know, they were in a car accident and they happen to have Parkinson’s disease. So this opportunity to kind of really focus on rehabbing the disease itself. It’s just been incredible.
Melani Dizon:
Oh yeah. That’s a really interesting way of looking at it. Well, I’m glad Jennifer came up with the idea, right? So, why did Dr. Elyaman stand out to you, Dr. Goldman when you were looking for candidates?
Jennifer Goldman:
Well, we were so pleased to have Dr. Elyaman as our first Fellow in the program and to kick it off with her joining our team for the fellowship this year, Dr. Elyaman, as she said, is just exuding passion and motivation and interest and initiative in this area and in this field. And I think that coupled with her fascination and incorporating principles of neurorehabilitation in the care and management of people living with Parkinson’s with her background as a physiatrist were just outstanding for her candidacy in the fellowship, and really bringing those elements to the field, working together as a team, engaging not only with the neurology community, but also the other rehabilitation professionals, whether physical therapy, speech language pathology, occupational therapy, and the whole host of rehabilitative services like therapeutic recreation and vocational rehabilitation and day rehabilitation, just putting it all together. It’s one big, big team that really focuses on function and quality of life and all those essential components to living with Parkinson’s and the care of people with Parkinson’s.
Melani Dizon:
Oh, that’s great. So, I wanna get down to like the details. So, Dr. Elyaman, what does a day look like? How are you getting sort of mentorship with Dr. Goldman, some other people at Shirley Ryan AbilityLab, what does your day-to-day work look like? And what are some of the things that have really stood out to you in the first six months of your fellowship?
Ala Elyaman:
That’s a great question. So, the days are pretty busy. Usually for example, on a day where I have a clinic where I’m working with both Dr. Goldman and Dr. Toledo, I’ll see maybe about five new patients in that day on its own. So, I’m able to observe not only the physician encounter with the patients, but I get to see the screening by the physical therapist, the speech therapist, and the occupational therapist. So, I get to kind of see all of the behind the scenes work in our two- hour visits, which is something that’s really unique about Shirley Ryan AbilityLab that we offer those two-hour visits. And then on days when I don’t see new patients, usually I’m seeing follow-up patients, either my own or with Dr. Goldman. And we kind of get to see after we’ve done therapies or, you know, depending on where they are in the course of their disease, how well are they doing, do they need a new course of therapy, are they doing well with their medications?
And just kind of getting to see the different stages of Parkinson’s disease, which has been really interesting as well. And then I also have the opportunity to work with some of the movement disorders neurologists that are at Northwestern. So that’s been really exciting too, because not only do I get to work with Dr. Goldman and I get the neurorehab side of treating Parkinson’s patients, but then I can see the purely neurology approach to seeing these patients as well, and kind of test myself and determine whether or not I’ve learned enough from Dr. Goldman to be able to talk to other neurologists that maybe aren’t as familiar with rehab care for these patients too.
Melani Dizon:
Right. Okay. So, when you have new patients coming into the AbilityLab and you have, it’s a two-hour session, are people coming to you in all stages? Do you find that you have more people sort of later stages like, oh gosh, like things are getting, I’ve had it for 10, 15 years, or, you know, what sort of people are you seeing, you know, mainly?
Ala Elyaman:
I would say it’s a good mix. Some that are just very early-stage disease, maybe just found out that they’ve been diagnosed. Maybe the symptoms were going on for a bit, but they didn’t realize what it was until they saw a neurologist. But then we are also seeing quite a few patients that have had Parkinson’s disease for a while, and maybe they just relocated to the area, or they’ve been managed by the neurologist and are suddenly realizing, you know, I’m having a lot more of a difficult time doing, you know, this, that, and the other in my daily life. And so, the neurologist is like, well, let’s send you to Shirley Ryan AbilityLab so that we can kind of get you tuned up and, you know, back in the game.
Melani Dizon:
Right, right. Yeah, when I think about this, oh, I talk to you and all I want is for every person with Parkinson’s to have this option, right. You just want them to be able to walk in and to have somebody like you and Dr. Goldman to see the entire circle of care that they could get and to make sure they get it all. And I certainly hope that from our standpoint that this fellowship is a massive success and that everybody gets this eventually. Right? What’s standing out to you, like what are you looking forward to in the next, the second half of this fellowship? Is there anything that you’re gonna do, that’s different, anything that you wanna point out that you’re excited about?
Ala Elyaman:
Yeah. So, I’m working on a research project at the moment. So, you know, trying to make sure that I have that done in my quality improvement project, which is more about kind of educating staff members, like the medical assistants on, you know, why it’s so important for us to understand what types of medications Parkinson’s patients take and why it’s important that we know the timing and the dosage, and, you know, what’s going on around the time that they are taking the medication. Are they taking it with food, you know, is it having the same as it used to? So that’s one thing that I’m excited about, you know, getting approval for and doing the research on that and seeing how educating them on these different things or the medical assistants, I mean, whether or not it makes an improvement in how we take care of our patients as well.
And then another new thing that’s actually pretty exciting and I’ve been able to kind of get started with in this second half of the fellowship is using osteopathic manipulation techniques on Parkinson’s patients as well. So, I was, I’m a DO physician. I went to medical school at Lake Erie College of Osteopathic Medicine in Erie, Pennsylvania, and was lucky enough to really get invested in osteopathic manipulation techniques and then to find an allopathic fellowship that allowed me to keep using those techniques is just fantastic. So, it’s been really exciting, and I’ve had quite a few patients that not only do they come in for the first visit, but then they make their next appointment on the way out. So that’s been really fun.
Melani Dizon:
You know you’re doing something right when that happens.
Ala Elyaman. Yeah.
Melani Dizon:
That’s great, that’s great. Dr. Goldman, what has been the best part of this experience for you, you know, and for Shirley Ryan AbilityLab?
Jennifer Goldman:
Sure. Well, this has been tremendously exciting on our end and my end to be able to develop a new program in an area that is certainly up and coming and growing, and really has not in some ways been done before. So, there hasn’t been a roadmap for this at all, and we’ve had a lot of fun in creating a curriculum for the fellowship, organizing what we’re calling core and specialty rotations of the fellowship that provide training across all the levels of care. So, I know we talked about our outpatient clinic here with interdisciplinary evaluations, but we span from inpatient hospital admissions for managing Parkinson’s symptoms, or if people are admitted for other reasons, our day rehabilitation programs, which are intensive day programs, but people go home to their own home at night, and then working with our outpatient rehabilitation therapists and other services.
So, it’s been really wonderful to be able to have this team approach and get everyone together from an educational standpoint. You know, I think there, no, there’s no better place to have done this here than at Shirley Ryan AbilityLab. We’ve been fortunate to be the number one rehabilitation hospital in the U.S. for the past 30 plus years since 1991. And there’s no better partner with whom to do this with Davis Phinney Foundation, as I think we’ve been really aligned in our missions of looking at how do we help people who are living with Parkinson’s now and their care partners and looking at their function and quality of life and team care and putting it all together. So, I’ve greatly enjoyed working with my colleagues to put the fellowship together. And it’s exciting to see it grow in traction. I think we’re learning from trainees and interests from people who are in residency and even medical students, that there is interest in this field, in Parkinson’s, interest from people living with Parkinson’s to access this type of care and research. And, you know, from my perspective, you know, thinking about how we build that pipeline of physiatrists, who can partner with neurologists and other healthcare professionals and train future generations to come.
Melani Dizon:
Yeah, absolutely. So that brings me, are you recruiting for another fellow?
Jennifer Goldman:
Yes, we are recruiting, and we are working to get the word out on this new program to the physiatry community, along with physical medicine and rehabilitation residencies and medical students. And then also raising awareness in the Parkinson’s community of how vital rehabilitation care can be in their journey with Parkinson’s from not only as we talked a little bit about very early stages, even at the time of diagnosis, but throughout the whole continuum and there’s great value that rehabilitation and physiatrists can play in their care. So, there’s always something we can do. It may look different at different stages of the disease, but I think that’s where our emphasis on function and quality of life are just so, so important.
Melani Dizon:
Yeah. So, I’d love to speak to that a little bit when you do get somebody who’s, you know, early in their diagnosis. And, you know, I suspect that they had great advice, or they got great advice from somebody else who has Parkinson’s or their neurologist and they said, hey, there is this sort of holistic approach, and you could check them out. What are some of the things that you do with them early on, ‘cause a lot of them, you know, ask us, why would I wanna do that? What do you, what can you do for them in those earlier stages?
Jennifer Goldman:
Yeah. So, I love that question. Because really it is a continuum and we’re trying to break the paradigm of traditional care, if you will, that, you know, where you see people who have run into complications, you know, such as falls or trouble swallowing, and then it’s only then that they get to see the therapist. So, we take a very different approach. We almost take the opposite approach. That one should be proactive in their care with baseline assessments. So, we do a lot of measuring of scales and ratings that we use to track people over time and look at outcomes and ultimately know is what we’re doing making that difference? So, even at very early stages upon diagnosis, having those assessments and gaining that education and knowledge about Parkinson’s and ways to be proactive are extremely important.
So, we do have a number of actually early intervention geared programs for people who are newly diagnosed on the role of physical therapy, occupational therapy, speech, language pathology, and also mental health and wellbeing to really see if we can set that trajectory and give people hope and optimism and tools that they can use to, you know, start that journey out in a positive element and then take that to reassess over time and set new goals and understand what can be personalized to that person’s needs at any given point in time.
Melani Dizon:
Right. So, do you have people that come, I guess I’m wondering if people, you know, fly in and come to the Shirley Ryan AbilityLab, do sort of that two-hour assessment and then leave and you are in communication with like their, at home PT or their home neurologist. How does that work?
Jennifer Goldman:
Yeah, so we do have a global patient services program here where people can come from wherever in the world, we’ve adapted with the COVID 19 pandemic and some travel restrictions over the past two plus years. But we are also able to offer telehealth services to do assessments by the physiatry physicians or myself and the team of physical therapists, speech language pathologists, and occupational therapists for an evaluation. And so, we do get people who will come in. We have people who will follow with us over time. We also work hand in hand with their local physician and healthcare team, which may include the therapist, may even in include their fitness instructor or personal trainer where we can have that dialogue about different recommendations. So, we’re very flexible in our approach. We work hand in hand with many movement disorder neurologists locally and beyond and really that holistic philosophy, this takes a team, it takes a village, so.
Melani Dizon:
Yeah, that’s great. Well, so, this is the big question here. Let’s say this program like fulfills your wildest dreams. What are your hopes for it going forward?
Jennifer Goldman:
Yeah, yeah, well, I think we are already off to a wonderful start and it’s so exciting to see it blossom and from, you know, an idea stage that I know we talked about once upon a time with Davis Phinney Foundation and an idea, and then actually to see it in action with Dr. Elyaman and I would really love to see this as the beginning stage of, as I said before, setting that pipeline. So being able to have physiatrists in the community, across multiple communities in the U.S. and beyond who are well-versed, well-educated and trained specifically in Parkinson’s neurorehab. So, they can then take care of the Parkinson’s community in their area, train other healthcare professionals and therapists, and really, you know, grow this and scale this beyond. I also think there’s a great interest and need to have more research in understanding physiatry and the rehabilitation role in Parkinson’s and bringing this, you know, into the global community. So, we have some global rehab initiatives underway and really just emphasize how we all can partner together in the care of someone with Parkinson’s and their caregivers and the role that rehabilitation can play coupled with neurology and all the other subspecialties together.
Melani Dizon:
Great. Well, thank you so much, Dr. Goldman and Dr. Elyaman. I really appreciate you guys being here to talk about it. We have been so excited, and I feel like I’ve been waiting for this conversation for years. So, this is great. I’m excited to share it with everybody and we will definitely be in touch toward the end of your fellowship to see what you’re gonna be up to next.
Additional Resources
To read more about Dr. Elyaman from the Shirley Ryan Ability Lab, click here.
To learn about Shirly Ryan AbilityLab’s Parkinson’s Disease and Neurologic Rehabilitation program, go here.