Introduction
Studies show that between 60 and 83% of people with Parkinson’s report experiencing pain, and chronic pain is twice as common in people living with Parkinson’s than it is in those without Parkinson’s. Several different types of pain are associated with Parkinson’s, and effective management requires coordination with your care team and implementation of pharma- and non-pharmacological treatments. In this primer, we address common questions about Parkinson’s-related pain, including types of pain, treatments, the pain ladder, and which specialists to see. Although many types of Parkinson’s pain are chronic, you can improve your quality of life and live well with Parkinson’s by taking control of your pain management plan.
What are the different types of pain experienced by people with Parkinson’s?
Five main types of pain are common for people with Parkinson’s. Multiple types may be present simultaneously or occur at different points throughout a person’s path with Parkinson’s. Recognizing which kind of pain is present can help you optimize treatment, as can paying attention to what activities or times of day make your pain better or worse.
Musculoskeletal pain
Musculoskeletal pain that affects muscles, bones, tendons, ligaments, and/or nerves. The pain can be localized or generalized and can fade or intensify at different times. Existing musculoskeletal pain can be exacerbated by Parkinson’s.
Neuropathic pain
Rather than being caused by a physical injury, this type of pain is caused by damage to the somatosensory nervous system or a disease affecting the somatosensory nervous system, which responds to external stimuli like touch, temperature, and vibration. It tends to be fairly consistent throughout the day and is present no matter what activity you’re doing. Unlike the aching you may feel when you’re doing a strenuous physical activity, neuropathic pain feels more like a tingly, crawly, uncomfortable sensation.
Dystonic pain
Dystonia, the movement disorder in which involuntary muscle contractions cause repetitive or twisting motions, is often very painful. Many people with Parkinson’s experience dystonia as a motor symptom, whether it’s localized (focal dystonia), in multiple nearby body parts (segmental dystonia), or all over (generalized dystonia).
Akathisia
This movement disorder is characterized by the inability to be still. Many people who experience it feel restless or uneasy and exhibit motions like pacing, rocking back and forth, or fidgeting. Often, if it affects a particular body part, it can cause sensations of burning or pain that can sometimes be relieved by moving that body part.
Central pain
When there’s damage to or dysfunction of the central nervous system (CNS) from causes such as a stroke, tumor, epilepsy, or Parkinson’s, central pain syndrome can be a result. The pain is usually chronic and constant and can affect a specific or generalized portion of the body.
How is pain treated for people with Parkinson’s?
No matter the cause, pain is often complex. When a person with Parkinson’s experiences intense pain, especially in combination with other symptoms of Parkinson’s, managing it can be challenging. There are, however, several ways you can adjust your medication regimen, exercise schedule, and lifestyle to reduce your pain and improve your quality of life.
Medications
There are various kinds of medications used to treat pain, especially for people with Parkinson’s. In a recent webinar, Dr. Janis Miyasaki described how physicians approach pharmacological treatment of pain for people with Parkinson’s:
The principle is to start with what is called the pain ladder. You always start with the least intensive, least side effect-giving treatment.
Janis Miyasaki, MD
Step one
The first step of the pain ladder is hot and cold treatments along with stretching and flexibility exercises. People who experience rigidity and stiffness can sometimes alleviate pain using heating pads to loosen their muscles, then improve mobility by stretching, then address any residual pain with ice packs. (And remember, especially if you’re new to daily exercise and have been more sedentary for a while, build your momentum and fitness levels slowly to avoid pain from overworking your muscles. Exercise is a cornerstone of living well with Parkinson’s, but stretching and improving your flexibility before you begin a more intense regimen can help you stay active without getting hurt.)
Step two
The next step on the pain ladder is low-dose, over-the-counter medications like acetaminophen and ibuprofen. Because these pharmacological interventions are relatively inexpensive, don’t require a prescription, and can be managed by the person with Parkinson’s, they are a great next step for the treatment of pain. If acetaminophen and ibuprofen aren’t doing the trick, transitioning to stronger non-steroidal anti-inflammatory drugs (NSAIDs) like Naproxen or Aleve may help. Remember to let your care provider know if you’re taking any medications, even those available over-the-counter, in addition to those they have prescribed.
Step three
The following step on the pain ladder is anti-depressants. Although using anti-depressants for pain relief may seem strange, medications like tramadol, tramacet, duloxetine, and many tricyclic anti-depressants are often used to treat pain in people with Parkinson’s when options on the lower steps of the pain ladder haven’t worked. However, these medications require more careful balancing with other medications. (For example, MAO-B inhibitors should not be taken with tramadol.) And because anxiety and depression are common non-motor symptoms of Parkinson’s, you may need to adjust your existing anti-depressants before starting new ones to manage your pain.
Step four
The next step includes anti-epileptic medications like gabapentin and pregabalin (the former is used off-label to treat pain while the latter is often prescribed to treat neuropathic pain specifically). Though there is limited research about these medications’ effectiveness in treating Parkinson’s-specific pain, they have been found useful for treating fibromyalgia pain, diabetic pain, and nerve pain; so, they may be appropriate medications if less intensive treatments have failed. However, be aware that doses high enough to effectively treat pain can also cause sedation, unsteadiness, and increased fall risk. Discuss their use with your care team.
Step five
The final step on the pain ladder is opioids. Many physicians refrain from prescribing opioids due to their addictive qualities and the potential for abuse, but if no other options on the pain ladder have been effective, you and your doctor may consider them. Studies have shown varied results about the efficacy of opioids for the treatment of Parkinson’s-related pain, so talk to your doctor about what the best treatment course might be.
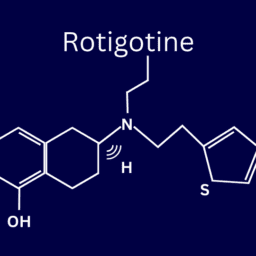
Other medical interventions
Other medications used to treat Parkinson’s pain include levodopa or dopamine agonists. Because levodopa lessens dystonia and rigidity (both of which can cause pain), your doctor may address your pain by increasing your dosage or the frequency at which you take levodopa. Other common interventions to address pain include Botox injections, surgery, or deep brain stimulation (DBS). Though CBD is sometimes touted as a cure-all for many Parkinson’s symptoms, including pain, studies offer conflicting evidence about its effectiveness . Be sure to work with the members of your care team to explore all your options and decide what might work best for you.
Non-pharmacological interventions
There are many steps you can take to manage your pain that are not medication-based, and lifestyle changes are often very effective. Complementary therapies and interventions like massage, stretching, yoga, increased amounts of exercise, heat and cold treatments, and physical or occupational therapy can help lessen your pain and improve your quality of life. It’s also important to eliminate (or at least minimize) activities and behaviors that can increase your pain. Consider making changes to your environment that will make your life more enjoyable, such as investing in more comfortable furniture or sitting rather than standing on public transport. These small lifestyle changes can have positive effects on experiences with pain.

Who should I see to discuss my Parkinson’s pain?
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist (MDS), start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain; so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinson’s-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no one’s path with Parkinson’s pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
What can I do on a regular basis to manage my pain?
Remember, you’re your best advocate as you understands how your pain feels. Understanding and communicating the kind of pain you’re experiencing can greatly inform your treatment plan and will allow your doctors to address the type and severity of your specific pain. Keep your care team informed about activities that cause pain or the times of day your pain is worst so they can help fine-tune your care plan. Do you notice the pain starting to creep in at a certain point after you take your medication? Do you feel fine when you bike but experience pain when you jog? Did you start experiencing this pain before or after your Parkinson’s diagnosis? Taking stock of these sorts of questions can be helpful as you work with your care team to effectively treat your pain.
Incorporating approved medications and following the pain ladder (only moving to more intensive treatment when necessary) can also help you find the right pain management solution, as can taking steps in your everyday life to be an active participant in your own pain management. Regular stretching, heat and cold treatments, exercise, yoga, and dance can all help reduce your pain, and they are all steps that you can take on your own. Making adjustments to your home and workspace, such as minimizing places where fall risks are likely, using an ergonomically designed desk, sleeping in a comfortable bed, and wearing clothes and shoes that don’t exacerbate pain, can help you establish a more pain-free daily routine.
And remember to ask for help when you need it. Even though you’re the person feeling the pain, involving others in your pain management plan is important. Getting your care team of physicians, mental health specialists, and care partners involved is tantamount to effectively combatting Parkinson’s pain.
To download this post as a PDF, click here.
More Resources
A Resource Guide of 19 Complementary Therapies for People With Parkinson’s
Anxiety, Marijuana, and Pain in Parkinson’s: 10 Expert Answers to your Hard Questions
WANT MORE PRACTICAL ARTICLES LIKE THIS?
Much more can be found in our Every Victory Counts® manual. It’s packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action. Request your free copy of the Every Victory Counts manual by clicking the button below.
Thank you to our 2020 Peak Partners, Amneal and Kyowa Kirin, with special support from Adamas, for helping us make printing, distributing, and shipping the Every Victory Counts manual possible.