[NOTE: Have a topic you’d like our YOPD Council to discuss in future sessions? We want to hear about it! Let us know what’s top of mind or any questions you’d like to ask panel members by filling out this form.]
During this session, our YOPD Council leaders answered YOUR questions, including their thoughts on topics including:
- Finding meaning and purpose in your life post-diagnosis
- How to deal with the highs and lows of living well with Parkinson’s
- Tips on medications and deep brain stimulation (DBS)
- Finding community and building support systems
You can listen to the podcast below.
You can read the transcript below. To download the transcript, click here.
(Note: This isn’t a perfect transcript, but it’s close.)
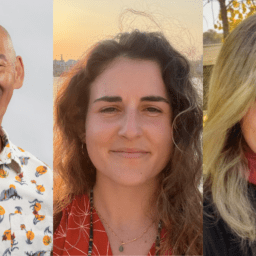
Melani Dizon (Director of Education and Research, Davis Phinney Foundation):
All right, my name is Melanie Dizon on the Director of Education and Research at the Davis Phinney Foundation and we are here today for our YOPD Council are super happy to have all of you here today.
So today we’re going to do some Q & A. And the reason why is because we’ve had a lot of requests for people to come on and just be able to ask questions, and then also I’ll invite our panel members for you guys to share what what’s top of mind for you if you think there’s something that we can share with the rest of the audience. Kat go for it.
Kat Hill (Davis Phinney Foundation Ambassador, YOPD Council Leader, and YOPD Women’s Council Leader):
So, one of the hardest things for me about being diagnosed young, is that I’m married to an equally young person, my husband Ken, and he is not near retirement or we didn’t think he was near retirement, and I think having a lot of time and feeling somewhat retired even though I’m, I left on medical leave and on disability. I’ve really missed being able to spend some time with him and so we’re currently exploring some options about ways for him to retire early so that we can maximize our time together in my healthier times. I’m noticing progression of symptoms, and I think a lot of us feel a clock ticking with a diagnosis like Parkinson’s, and I feel excited and a little nervous about looking at options. So, that’s kind of where I am at the stage of life and I don’t know that we’ll be able to do it but we’re looking at things like selling our house maybe and doing some traveling in a trailer. A little air stream maybe, I don’t know, we’ll see. But, but it’s a big change, a big change in a time when we didn’t think we’d be dealing with it in our 50s rather than later. So, it’s more just something to report, and I’d love to hear what other people have done out there and and ways they’ve looked at it and any advice for us as we’re looking at options, so I’ll open that up to the panel for sure. And anybody else at home that can chime in.
Kevin Kwok (Davis Phinney Foundation Board of Directors member and YOPD Council Leader): I’m a strong endorser of car top campers.
Kat Hill:
Can you get in and out, Kevin? Is it hard?
Kevin Kwok:
You know what it’s part of my occupational therapy getting in and out but I love it, it’s it’s it’s my freedom machine and we just during covid we used it, it’s sort of an in between step of selling your house and buying an RV or you know, one of those sprinter vans. Yeah, the freedom of seeing things and experiencing things is wonderful.
Kat Hill:
Okay, I’ve seen your pictures Kevin and they’re impressive but I keep thinking how am I gonna get up there?
Karen Frank (Davis Phinney Foundation Ambassador, YOPD Council Leader):
Kevin how do you go to the bathroom and how many times a night you have to go to the bathroom?
Kevin Kwok:
Just cut your wine and beer intake before going to bed.
Tom Palizzi (Davis Phinney Foundation Ambassador, YOPD Council Leader): It’s one of those you climb in and fall out kind of things.
Karen Frank:
I think you should have a fireman’s pole that you can slide down
Kat Hill:
Or an inflatable slide, like the inflatable slides is what I was thinking more. Yeah, I like that Kevin though thank you that’s an endorsement.
Melani Dizon:
That’s a good idea. Also, you should check out the camping series right like they had some really awesome tips on that was fun.
Tom Palizzi:
If I could quickly offer something to Kat. When you do things with your husband in this period, that’s forthcoming exercise together is always good for both of you, so that’ll keep you going you know keep him going so make that a big part of what you do so, I think that’ll be good.
Kat Hill:
Yeah we’ve been building that in already, I just look forward to having him a little more after exercise.
Melani Dizon:
I’d love to you know go a little bit into this topic because I think there’s like the logistical piece of retiring and there’s doing the financial assessment and doing the home assessment all of those different things.
But for those of you who have retired whether intentionally or not intentionally. There’s also that feeling of purpose and meaning of getting up and feeling like what am I doing now I’m not, I’m not, I’m not working. Or like I don’t have the same identity as a worker as I used to. What do you do with that? How does that feel? What are the challenges and what are some things that you’ve done to, you know, find the purpose and meaning elsewhere? I mean, aside from being here which is a big deal. So, yeah. Anybody have any thoughts on that, Karen?
Karen Frank:
I remember where I where I’m at three or four years into my diagnosis is very different. Kevin was one of the first people that I met actually with Parkinson’s and I went on a Parkinson ski retreat because I love to ski and Kevin was on the ski retreat and I remember being very very depressed during that time it was during the first year of my diagnosis. I wasn’t working, I had been a nurse anesthetist and a busy practice, and my husband was very introverted and he didn’t really want to be on the trip now he loves his trip. We’ve gone back before but it was a hard time for us. And I specifically just Kevin shined so bright. And I remember feeling like I wanted to feel the way he looked, I wanted to feel the way on the inside that he looked on the outside.
And I remember asking him about it and he told me about his talk about mindful pivoting, and when he made the, which is one of the Davis Phinney talks that he had given and when he made that sort of transition from making that decision that, that this could be a positive thing in his life, to have that Parkinson’s diagnosis, and that talk really turned things around for me. I remember, okay, I can do this I can go back home and I could do this and somebody put a question in the chat about how did they meet other people with Parkinson’s and I enjoyed so much as much as I hated being around other people with Parkinson’s at the beginning I also enjoyed it, and it was sort of like, I was drawn to it but I wasn’t sure why, and how and I just slowly started building a new life for myself and bit by bit, it just got better and better and now I can truly say I am a much happier person now with Parkinson’s four years later than without Parkinson’s before, it’s just really illuminated my life.
Melani Dizon
Thank you. That’s great Karen.
Heather Kennedy (Davis Phinney Foundation Ambassador, YOPD Council Leader):
And to add to that I don’t know that I would say I’m a happier person, but I’m more humble. I’m more interested in spiritual, just everything is taking the trajectory of away from the material world and into the spiritual for me.
And I write more, I think with more depth. And I want my relationships to have more intimacy and depth, because I’m playing for keeps now, whereas before I might have thought that I had time. And as you can see I don’t I don’t believe I have time anymore, you know, this is says and Latin remember you will die which is to remember to live right now to sort of bounce off what everyone has said here in our introductions, like Kat, we need to stay here now, and that’s that’s the hardest thing for me to let go of that grasping onto the past and the future and try to stay here now, because the ego is always looking for, you know, a job, perceived threats and to be worried, but the stay here right now is what we’ve got. It’s what we’ve got, you know, so for that I am thankful.
Kevin Kwok:
Yeah, no you know your comment on retirement and resignation is particularly true for me because I actually just got my termination, my official end the word termination letter yesterday, wow, and it really stung even though I kind of admitted to myself that it was time to stop working.
And it was I think so much of our self-worth unfortunately is placed in work falsely so. And while you know I’ve constantly felt like this is my new job now right, taking care of myself and taking care of the tribe. It hurts when you get that letter and you actually sign it, you know, and I don’t know how others in the panel have dealt with it but I think we ride this roller coaster through highs and lows all the time. Sometimes daily sometimes weekly but we all have that cycle.
And I had sort of built up this idea that, you know, retiring at 60 would be a great thing. And I still think it is, but I still go back to what about all those zoom calls, what about all those trips that I used to make for work, what about all the meetings I used to prepare for and I just have to kind of move off that.
Melani Dizon:
Absolutely. Amy, you were going to jump in.
Amy Montemarano (Davis Phinney Foundation Ambassador, YOPD Council Leader):
I was going to jump in as the counter voice I guess to Kat because I am not yet at a place where we can make those decisions. So, I’m holding on for dear life to the working world.
And if anybody is in that same space, I’m happy to talk to them elsewhere but I am, yeah, sort of like, those aren’t those aren’t options right now so there’s plenty of us I think that fall on both of those lines, and, and, for anybody who’s trying to not retire, because they either don’t think they can, or they literally can’t. That’s another it’s another topic, too.
Melani Dizon:
Yeah, absolutely. Absolutely, yeah and let us know if you guys want to reach out and we, you can look for Amy on our site and I know should be perfectly happy to talk to you.
And then also, Tom Cosentino one of our ambassadors said that, I’ll get to your other question too Tom, but he said he also we sold our house and moved to Delaware I have enough funds to now be retired and my wife will be retired in two years. I’m a numbers
guy and willing to talk to anyone on this, so thank you so much Tom for offering that I’m sure people will take you up on it. Tom, what did you, what were you going to say?
Tom Palizzi:
Basically what time the other Tom just said, we actually know each other. We’ve talked to each
other on the phone.
I’ve been through the diagnosis, and I worked for about four or five more years following that, I did a year transition out of work and I’ve been retired ever since. I’m dealing with this for 13 years. I’m certainly open to talk to people about it and there’s, there are some very identifiable steps and then there’s a lot of things that are not not quite as identifiable so some intangible things that you can deal with but again I’m more than happy to talk to people about making that transition both from work, to retirement as well as how to redefine yourself and how to set a new game plan for that you didn’t plan on doing to begin with. So.
Kat Hill:
Yeah, and I think that’s what I’d like to add that, that part of why we’re looking at it is about a time issue not about we’re having to kind of right size our life in a lot of ways, which we’ve had to do, which will mean downsizing and shrinking what our expectations are, and valuing time together perhaps more than things and cars and big trips or getting creative about it, I’ve talked about that before, that I had always hoped to travel in retirement and without an income that has been very difficult for us. So, we’ve gotten creative, sharing, you know doing house trades and building up points and renting out some of the space in our house so I think that, I think that with the right mindset and congruent priorities in a team that you can find a middle place because the last thing I wanted to do is give up my career, delivering babies. It was a great career, and I feel like I’m in the second act now, and I’m focusing on the things that I can do, and trying to let go of the things that, that are more difficult or hard or more challenging and trying to focus on like Heather relationships and people and playing for keeps.
Yeah, none of us plan this right Kev, right, so you know we all think oh, we’ll work till 65 or taper off the kids will be through college, I still have, well one just graduated I still have two kids in college so it’s about getting creative for us and thinking outside the box and living with less, frankly. And that’s not all bad less is not bad. Less is sometimes really simple, which I love.
Melani Dizon:
So right yes so as Heather said this is not what we had planned so letting go and and reimagining our careers is our constant transition.
Yeah, I mean I think it does take it takes a whole just reframing this, it is this thing and there’s no fighting it, there’s no taking it back so what what can be done. Let’s see we have a lot of questions. Yvonne said retiring early has been the bomb, it has been opportunity in many ways. Yes, we did put some info about the ski trip and we also put Kevin’s talk up there so if you don’t get it here, you’ll get it in the show notes for sure.
I just want to make sure and go back to some of the questions. Oh, Heather, actually, let’s go to Heather, Heather DBS. What are you open to sharing? And whatever that is, we would love to hear about it, we’d love to hear about you know the decision what made you decide to do it, the surgery itself and then what would have been the after downstream impacts of it.
Heather Kennedy:
Well, as many of you know, including Davis, at a certain point in time you drugs, lose their efficacy and so you run out of choices and you find yourself in a dystonia, or you might have bradykinesia and dystonia, you might have, you know, a lot of other things, I had the dystonia and the bradykinesia and so I was really upset that I was not able to function anymore.
And I’ve been so disappointed with my programming, until you guys are not going to believe this is why they need to do more tests on women, I took off my Combi patch for menopause and my drugs work again. And the DBS suddenly works.
The Combi patch blocked the drugs from getting into my system somehow I do not know why there are no I can find no studies to confirm this, but that’s the only change that I made medically, I have the same exact lifestyle, same exact meds, same exact diet, sleep pattern, everything’s exactly the same, I haven’t even changed my relationships or anything, there’snothing going on in my life that would be starting at all. But upon taking that patch off within a few days, the meds work again, look.
Melani Dizon:
Wait, so wait, what made you think to take the do the patch, take the patch off?
Heather Kennedy:
My doctors, thank goodness because I had been hammering, I mean really hammering the people that are on my team. Every day I was like texting them saying I can’t move. I’m afraid it’s I feel like I’m at the end of my life, a palliative care couldn’t get down the stairs. I was slurring except for maybe one or two hours each day when I would become manic after taking a lot of drugs for the Parkinson’s medications and and I couldn’t figure it out, we just it was a process of elimination.
I’m already dairy free, you know wheat free I’m very careful with my diet wasn’t that, and I tried not to eat during my medication I’ve tried everything, everything and removing the combi patch which is an estrogen patch for women that are going through menopause. Everything seems to be kind of okay.
Melani Dizon:
You won’t find that in a book or a Parkinson’s resource or anything.
Heather Kennedy:
You heard it here first kids.
Melani Dizon:
Yeah. So that’s truly amazing so you’re, you’re feeling great today?
Heather Kennedy:
Yeah. And just to be specific about this I did the globus pallidas, not the sub thalamic nucleus
like Benjamin Stature had a different, you know, insertion place so the biggest challenge is the globas pallidus is the size of the Jelly Bean roughly it’s a little bit harder to program a little more complex it’s a very if you do get DBS of highly recommend, try to be patient. I hate that word, like don’t tell me to be patient when I can’t even bathe myself or cut my own food, you know, don’t, don’t tell me to be patient. But, if you can be patient and wait out your programming, it will behoove you.
Kat Hill:
Heather how long has it been since your surgery?
Heather Kennedy:
When were you over, three months, or four months? Yeah.
Kat Hill:
Yeah, thought people should know your timeline.
Heather Kennedy:
Yeah, about four months in, and I was ready to throw in the towel I mean I was like, this is the end of my life. I’m quitting all my jobs. I can’t hear myself and my family, I was truly losing hope for the first time in my life I was devastated. I thought I made a terrible mistake. I’ve had MRIs to check everything and it’s all good so far.
Melani Dizon:
Wow, that’s great. very good news, very happy to hear that.
Heather Kennedy: Thank you.
Melani Dizon:
Speaking of drugs. The question is, does anyone, has anyone did anyone delay starting drugs? So you know our general advice and general advice from our doctors are, you know, the minute it starts impacting your daily life impacting, you know, daily activities going to the bathroom getting coffee any of those things anytime it starts impacting that’s a good time to take them. But if anybody here delayed it and wants to speak to that, Kat.
Kat Hill:
Yeah I waited.
I was concerned about the side effects of dyskinesias and, and I hadn’t read a lot of evidence that supported starting meds early. However, I think that’s changing I think there are more studies out now that seem to share that we might have window of time where it’s the most efficacious for us to take medicines. I wish, in retrospect I wouldn’t have waited so long.
And, but I also don’t believe in regret. I believe that you make the best choice with the tools you’re presented. I waited about three years before starting Sinemet. And about two years before starting the agonists, but I felt better pretty quickly after starting the medicines. So, but I have gone up fairly quickly in my dosing probably to catch up with disease progression. And you know that that was my reasoning, and yet my baseline was if I couldn’t get out and go exercise and exercise hard that I needed to be on medicine and when that the dystonia started to really affect that that’s when I started.
Melani Dizon:
Great. And I can’t tell if you’ve already done that Leigh but if you could put that medication, those two webinars with Dr. Aaron Haug in the chat, people will get it we did a general one and then we did Q & A and that’ll be really great. Tom and then Kevin.
Tom Palizzi:
Yeah, thank you Heather, um, I started out quite slowly at the advice of my doctor and back in those days again this is 13 years ago that was kind of the more of the common thought although in the few years after that I started to see things change to where doctors were starting medications earlier.
Now it depends on a lot of things like how severe you might be when you start or when you were originally diagnosed versus how you may not be showing any symptoms like I didn’t have a tremor, so I didn’t have to have much under control so to speak with the medication so that helped me to stave off the use of medication for quite a number of years, and then gradually I started on with agonists first, then carbidopa/levodopa and that’s all I’m still taking today, so. And not that much comparatively speaking about six to seven pills carbidopa/levodopas a day, about every four hours.
Melani Dizon:
Okay, great. I have another question for you, Tom related to that but we’ll, let’s go to Kevin first and then we’ll, okay.
Kevin Kwok:
So, um, you know, in my case I actually wanted the early confirmation that my diagnosis was correct. And I sort of assumed that if I reacted to Sinemet that it was a true Parkinson’s diagnosis. But that was actually a slippery slope because once I started that, then they started adding on dopamine agonists, which I would say work for some but take with great caution if you have young onset because of some of the behavioral changes that I experienced, and I know many of you, others have experienced as well.
Yeah, I think that the one thing that for me was just the light of my journey was that when I had DBS I actually went medication free for four years. So that was blissful because not only was DBS working, I was exercising like a feen, but I didn’t have to take medicine which was wonderful. And I’m a pharmaceutical guy so you know for me to say that medications were actually a negative thing is quite an enlightenment.
Melani Dizon:
Yeah. Okay. So Tom. I think we did talk about this last time about dyskinesia during exercise you remember that? Okay. So this question is, the person says when he takes a half a carbidopa/levodopa to mediate an episode how long does it take to become effective and what, what do you do during that time? So I think you usually take it when you’re exercising if you need more right like during it or, but right before it?
Tom Palizzi:
You know, I don’t usually take additional unless for some reason I’m suffering more longer periods which I don’t typically do. So I’ll take two Sinemet, and a Comptan as part of my regime, and then I’ll, if I need to take more if I’m going to be exercising like the other day when we were running to tour to victory bike ride. I wasn’t riding but I was, I was working the whole day. I took a bottle, a solid-colored bottle so it doesn’t let light in, and I’ll a Sinemet in that bottle.
And then as I drink from that bottle water all day long. I’m always getting a little bit of Sinemet just to keep myself kind of topped off during the day and that works absolutely wonderfully so that kind of takes out the dips in the OFF periods. And, I come ON much quicker than normal.
Melani Dizon:
Okay, thank you for that. That’s really good health. Karen did you have your hand raised?
Karen Frank:
So make sure, yeah, I’m kind of circling back to the medication question at the beginning, I actually went on medication right away and I had a lot of problems with the medication, everything from severe nausea, to the levodopa to side effects from the dopamine agonists causing severe impulse control problems for me, and drug reactions with some of the other medicines like the rasagiline and I just really struggled I tried very hard to take the medication.
I decided at the beginning that the medication was, the treatment was worse than the disease for me. And I actually chose to go off the medication for a period of time, and focus on exercise, mindfulness, meditation, things that would actually improve the quality of my life, not detract from the quality of my life and my neurologist, said you know when you’re ready, I actually considered early deep brain stimulation and decided at that time to hold off.
I decided after about a year off medication to give it a try again, because I really felt that taking levodopa was going to be important for the quality of my life with Parkinson’s disease. And when I did it again, I had success, and really just taking some steps away, maybe the anxiety of the early diagnosis was contributing to the side effect profiles of the medication so I kind of started on it, went off it, and then went back on it again and and and that worked for me, so I it was something a little different than some other people might have so I wanted to share that with with you guys.
Melani Dizon: Thank you. Kat?
Kat Hill:
I just wanted to advocate that that people out there, sometimes you think if you start a medicine you can’t stop it and it’s certainly important to work in tandem with your provider and whoever’s prescribing it, but you really get to be the boss of what’s going on with you, and it’s, you pay people that you go to see your providers, your pharmacist, your occupational therapist, your massage therapist, you’re paying money and you’re the consumer and you get to make the decisions that are right for you and if something isn’t working, it’s okay to be the squeaky wheel and to make phone calls and to say I’m not feeling good, and I’m not sure this is working and and it’s okay to go off a medicine right Karen, you know it’s you do it in tandem with your provider.
You know, Heather just talked about stopping a medicine, Karen talked about it. You have to partner with your providers and and the people that you trust to give you information, but it’s ultimately your decision about how you manage it and I think sometimes we forget that that that we, we are the captain of the ship, we’re the, you know, where the chick in charge and or the or the or the guy that the chunk in charge, however you put it.
Melani Dizon:
Thank you. Um, this is a great question. I think this is going to be. I think everyone’s going to have something about this so here’s the question, what do you do when your soul gets tired of fighting this every day?
Kevin Kwok:
You know it’s funny, this is a question that I wanted to raise with the group too because I was just on the road visiting a fellow ambassador in Nevada. And he was telling me that, you know, he’d hit the wall and was thinking, suicidal thoughts.
And I promised him that we would discuss this issue because the issue of mental health, and the dark days or something that hit many of us. I mean I’ve, I’ve certainly been there as well. And I think we all need to find, two things, one how we deal with it with ourselves, and how do we help others express it to us. So I don’t have all the answers, but I do know that social interaction and being and knowing that you’re not alone in your journey has helped me, helping other people has helped me too.
So those become sort of mechanisms, but it’s not always easy just being a cheerleader right. I think we all get weary of there from time to time. And we just have to forgive ourselves, when we do take a lull and find whatever it is medication, meditation, you know, travel escape, whatever it is you do. We just have to find our own cycle of how to pick ourselves back up. I’m curious how my other panel members pick themselves up.
Tom Palizzi:
That that’s a really, really good response Kevin. You know, I think, Davis Phinney said it best, and how I’ve always kind of put it away in my mind is that it takes courage to have Parkinson’s disease. And it takes even more courage to live well with Parkinson’s disease. So I think those words have always echoed in my mind whenever I felt a little despair little discouraged about, you know, my day and I just, I find myself wanting to do that little bit more when I feel like I can’t, and that always seems to bring me around and that’s not a cure for everybody by any means but the other thing is, depression and anxiety are not something you should try to take on yourself, by yourself I think you need to get, not just professional help but help from your friends and peers and this group for example we’re certainly available to help talk to you at least and so again it’s easier said than done, but we’re here.
Melani Dizon:
Thank you for that Tom, Heather?
Heather Kennedy:
What I find really helpful is to keep asking the questions and being curious about why you’re suffering so, instead of wanting that quick immediate release to get out of your suffering. I know this is really hard to say. And it does not apply necessarily to someone who’s suicidal.
But to stay in it and to remember it’s temporary. You are grounded you are, you have a reason to be here. You are necessary on this planet, and with your family and the people around you, whether or not you feel that is not really up to you, you, you need to be here.
You do grounding meditation you can ask for help. You can also be in service, one of the fastest ways for me to get out of my downward spiral is to help somebody else. And when I say help somebody else, someone who’s asking for help.
I don’t go looking like “Does anybody need some help? Would you like my opinion?” You know it’s not like that it’s more like there’s something called the soft white underbelly that I listened to on YouTube. It is a man who interviews people who are really down on their luck, the forgotten people in the world. Addicts, people that live on the street, a lot of homeless people.
And I don’t take strength from it, but I am reminded by it that it can always be worse. And also when I’m really really low I remember all the people who’ve given me love all the ancestors who work so hard to get me here, and never give up.
And yes, of course, reach out. And when you do reach out don’t expect someone to always be, or do the right thing, because you know we’re not trained either we don’t really know nobody knows what to do.
You don’t know how you’re catching someone like you might catch them the middle of something, and they’re very nonchalantly kind of, you know, kept push your question off. It’s not personal. We’re all very distracted by our own stuff, just, you know, try to return to that place of it being impermanent, whenever possible. It’s impermanent, it will pass I promise.
Melani Dizon:
Karen, and then Amy.
Karen Frank:
I’ve struggled with depression in my life before Parkinson’s and I don’t know if it’s a neuropsychiatric complication of Parkinson’s or just something that I’ve contended with, you know, my father had Parkinson’s and I’ve talked to Heather about this she used the term before toxic positivity, it’s, you know, it’s not real. Nobody’s positive all the time. And, you know, the other day I had to go off my levodopa for 48 hours for an exam, and I mean I thought I wanted to jump from a building, I’m not exaggerating, I was very dark I was very depressed, I did not feel well, and I didn’t recognize it was happening. That was the scariest part.
I was writing a poem about it and the poem was very very dark and I shared it with because I’m in a poetry group I shared it with my brothers, and they called me, I even said on the email, this is like my last poem and I wasn’t saying I was, you know, was suicidal but I didn’t even realize the language I was using in my own head and they called me and they were like, are you okay, you’re not going to share that poem in your poetry group are you? And I was like it’s a poetry group. Yes, I am. But um, I didn’t realize it was happening and my brother who’s a physician said, is it possible that you went from 800 milligrams a day of levodopa to zero, and you’re having a side effect here.
And that never even occurred to me and I’m a medical professional, so I think having people around me who love and care about me and leaning into my friends with Parkinson’s that’s been critical because I don’t always want to lean into my husband for things, because it’s a heavy burden to bear.
I need another community around me, to help me, and I’ve connected enough because of the relationships I’ve built that I know I can call someone who safe, and I called Heather actually and she told me she understood, and that made all the difference.
But the other thing is, is reaching, you know, being in service to others, and we’ve heard this from a number of people, is huge and I learned that in AA, I’m a member of AA and leaning, you know, being of service to others is is just critical in life, to really kind of getting out of your own stuff and reaching your hand out to another human. To me that’s helpful.
Melani Dizon: Thanks Karen, Amy?
Amy Montemarano:
Yeah, I think we’re all saying the same things, and community and reaching out is really important, getting proper medical therapy for clinical anxiety and depression is really important.
And I say the same things and I frame it a little bit differently than Heather and Karen, but it’s the same exact thing. I tend to when I, when I feel down at tends to be at night. And invariably I feel better in the morning.
But, at at night, I try to just lose myself in something bigger. I tend to go into literature or some philosophy or just things that take me out of my own little self that helps. And it’s the same thing that that you all are talking about in terms of sort of seeing the bigger things that life is about than just your little problems and your little world.
And when you talk about service I talk about responsibility, I think, I think it’s really therapeutic to have a responsibility toward something that makes you get out of bed and have to do something, which is kind of, I think a little reason why I’m terrified of retirement, a little bit because I feel like getting up and having to go to work and take care of my children is keeping me well, and and that’s just like service.
And so responsibility with a capital R is a really big really big factor in wellness for me but I don’t know what it feels like to not have that, and I think I’m a little scared of that.
Melani Dizon:
Heather you’re muted, sorry.
Heather Kennedy:
There’s a great quote about that Amy, it’s by Victor Hugo I think, the peculiarity of of the sunrise, is to make us laugh at all our terrors of the night, and our laugh is always proportionate to the fear we’ve had, like the peculiarity of the sunrise is to sort of wake us up again, like, oh my gosh, the sun keeps rising. Because I get terrified at night too. I live alone.
Melani Dizon:
Heidi said I think my faith keeps me going being creative also helps. Yeah.
So this is interesting, Chris said I’m sure there’s a relation to these feelings and our dopamine levels, it actually hurts more on days that I hurt more, so it hurts, mentally, when I hurt physically, right? Did someone else, Karen did you have your hand up again, or
Karen Frank:
I was gonna say I’m on, you know I were never too old to learn things, and I learned something really major the other day about the way I approach, sorrow, and this was a really great lesson.
I’ve always done a gratitude list, and when I’m feeling down, I’ve done a gratitude list, and I would say, you know, some days it’s really hard to find something to be grateful for and something might be you know, I’m grateful, I can hear, I’m grateful that I don’t have a paper cut, you know I’m grateful I don’t have dystonia right this second.
Sometimes I have to reach for something but someone said to me, this and this is what really changed my viewpoint. They said it’s important to have a grateful list but it’s also important to have a hateful list, that you have to acknowledge both sides of that coin, you can’t constantly just be all Pollyanna about everything that’s wonderful because it doesn’t acknowledge that dark side and that that deep pain that we experience as humans living life whether it’s with Parkinson’s or just living life and I never thought of that. And it really just changed my view because my favorite quote I thought about it when Heather did is by Kahlil Gibran from the book The Prophet he’s a Lebanese poet and he says, the deeper that sorrow carves into your being, the more joy you can contain.
And it reminds me a little bit of Heather’s quote but you can’t have one without the other. And I think the acknowledgement of that pain and sorrow is important.
Melani Dizon:
So, somebody asked a great question, and it was gonna be my question so this is perfect. So a lot of what you guys have talked about today has to do with having a support group, having the people in your life having people you can call, people on speed dial, I’m having this issue, can you help me out.
I think it would be great to offer some really really practical steps that people can take. Yes, we’re moving out of covid, but you know what are both like what are some two, you know, whether you know back in the world, great things to do, or just at home things to do, what are some specific things that you guys did that really helped you build your friend with Parkinson’s network? Anybody want to? Kat.
Kat Hill:
So I think I’m remembering back to being early diagnosed and it took a little while to find a network of people for me and, and a support group. And, and I found kind of my people both at exercise classes and then starting a young onset support group, so I think giving yourself some grace, and then Heather’s favorite word, a little bit of patience to find your people. But, and to also accept that you might need to coexist a little bit in that uncomfortable space for a little while until you build that network, what I want to say is we’re all here.
The Davis Phinney Foundation is here. The World Parkinson Coalition is here there’s all kinds of organizations that you can reach out to now online or virtually. There’s ambassadors, we’re all, many of us are ambassadors, the Davis Phinney Foundation we’re available to talk and reach out if you are feeling alone so I think that’s the biggest piece.
And for me on those really really dark days, I have my go to phone call people who I will reach out to and and they’re a small handful of people but if I call and say I’m struggling they’ll call me back. Or I’ll text hey, I need you, and those are lifelines for me, and sometimes it’s my husband but like you, I think, Amy or Karen somebody was mentioning that you don’t always want to go to your partner or your care partner, all the time.
And because people, other people with Parkinson’s get it in a way that people without Parkinson’s don’t. So, all I can say is that none of us want you to feel like you’re out there alone.
That’s why we’re here doing this, and we’re accessible, we’re available if you’re feeling like you don’t have somewhere to reach out to. So, that’s my soapbox announcement I guess.
Melani Dizon:
Thank you Kat, Tom?
Tom Palizzi:
That was a good one. Good soapbox Kat, I totally appreciate it. Hey, I started kind of the same way, I got involved right away I started volunteering for the Parkinson’s Association of the Rockies here in Denver I just answered the phones on Friday mornings that’s all I did.
And that led to me, meeting some folks there and then going to support group meetings and whatnot. And that doesn’t mean you have to start one but you can I think that’s a great idea but just attending one.
And then at one of the Davis Phinney events years ago, I was just standing there and this guy just walked up to me we start chatting. And he said, Look, I don’t want to sound weird or anything you said but I don’t have anybody to talk to you all day every day would you like to go out for coffee?
Don and I are still really close friends today and we met by 13 years ago. So, just get involved.
Melani Dizon:
Yeah, yeah I mean I don’t know about you guys but I’ve never met somebody in this Parkinson’s community who I didn’t ask a question or reach out and they weren’t like immediately on it, and wanting to figure out how to help so if I were to get a chronic condition I would hope it would be this because I would know so many people that I can reach out to.
They’re just, it’s great. So if you are on this call right now and you are like I wish I was in that I wish I was one of those panelists they’re all friends they all know each other. You can you can be there we will help facilitate, you can email us at anytime and we are going to figure something out for you. You do not have to do this alone.
Amy were you just gonna say something?
Amy Montemarano:
Yeah, I just want a second that because I’ve gotten a lot of people contacting me through my role as Ambassador as everybody else has to and some people have told me that they were afraid because they were afraid to talk about it.
And so they resisted the call they resisted the email, because they couldn’t hear themselves, say that they had Parkinson’s, and I understand that feeling. And I want to just really encourage everybody to just make that call, send that email because I think that’s the biggest hurdle is hearing yourself say it, I have Parkinson’s and telling somebody else.
Once you say it, it opens up a lot of other things that make it a lot easier. And I heard Tom say that he was answering calls, when my dog died, I call the dog hotline for people who just lost their dog, and I was on the phone for three hours with that person.
And that changed everything, it was so helpful. And just a hotline like just, just make a call doesn’t matter really who’s hearing you. As long as they are sort of trained as we all are to sort of help you through this, please don’t be afraid to make the call. It helps a lot.
Heather Kennedy:
One of our attendees brings up an excellent point to about mental health having a stigma. Um, I’m going to go with this, and I know this is easy for me to say because I’m a person who has my basic needs covered, and I’m not fighting for a, keep my job, my main job.
But I want to say this about mental health. It would be a lot worse if you deny it, and try to put it in a box somewhere and tuck it away than go ahead and let it out a little bit. And I don’t mean to say that you’re going to walk up to everyone say hi I’m mentally ill. Hey I’m having troubles with this, but to acknowledge that Parkinson’s comes with almost always some type of illness that includes anxiety depression chronic mental health problems to deny that is to deny ourselves healing.
So I’d rather go ahead and say it take the chance of being judged and scrutinized and shunned than to ignore it and not get the help we need. So, and I’m, I’ll be the first one here to admit live right now that I do struggle with mental health issues, I do struggle with story lining and anxiety and depression, all the time.
I can feel it nipping at my heels, but the fact that I’m acknowledging it is very much like being in recovery and saying, I’m an alcoholic you know it’s very much like that to acknowledge it is why is how we start to heal. Just want to add that in.
Kevin Kwok:
Heather, I think that’s really great what you said, it is more challenging when someone is in the working world, because your colleagues as supportive as they are, will judge you, and you, you could see it almost instantly when you do disclose it that you’re having some issues is that all of a sudden the choice projects don’t come your way, or you get marginalized.
And I think it’s just that’s just part of the bigger picture that we have in our acceptance is that being marginalized, or as I call trivialized is just part of what comes with this right?
And you just find new ways of finding value and developing value and transferring value to someone else.
Melani Dizon:
Yeah, thank you, Kevin.
Also I mean you know you can one one way to look at it is you know you broke your leg, you’re not going to not get it fixed. You have an injury, mental health is nothing more than an injury, and you can get it fixed, you can get it worked on you’re like just like a, you know, I had 8000 knee blowouts it’s never going to be the same, but it’s better. It’s I’m getting it fixed every time I can, I’m doing the work.
And if you go for mental health help, it might not, you know, change everything but you will get the tools and you will become a skill builder and you will become somebody who can manage it.
So, yeah, I mean, nothing to be afraid of and also I mean everybody is here is telling you this is part of it. And if you have a good doctor, they know it too, and they’re going to help you find the resources in your area that can help you out. So don’t ever be afraid to, to bring it up.
We are coming up toward the end of the hour but I would love if there’s any last minute questions that anybody has or any last minute comments that people want to share, before we head out. Yes, exactly. We’re all just human beings after all, just with different brain chemistry absolutely right. Anybody else have any final thoughts?
Amy Montemarano:
I just have one quick one quick thing to add to this, I think that part of getting out of that fear, and that despair is feeling proud of ourselves and everything that you can do, and everything that you can show other people that you can do I think having some pride in your post diagnosis life is super important, and can get you unstuck fairly, fairly well.
Kat Hill:
Amy I totally agree. I think, you know, just showing up is a victory, getting out of bed is a victory. I’ve said it before and I mean, every day, the garbage getting taken is something to be grateful for, you know. So, yeah, you know, brushing your teeth some days that’s the biggest victory if you don’t have an electric toothbrush. So, um, you know, I think, I think we can find them if we look hard enough, we can find the things to be grateful for and the ways to coexist with Parkinson’s, and I’m really grateful for all of you here today, and I really thank people for showing up too and asking some questions.
Heather Kennedy:
I want to add we can look at each other like we’re all tallchildren because we kind of are we’re all just kids, muddling through.
Melani Dizon:
I feel like this is a fun time to offer two really fun pieces of advice on oral health since Kat just mentioned it today. So I learned two things for people with Parkinson’s this week on keeping your mouth healthy which is crazy important, and we’re going to be offering some info on that but one of the things is when you have an electric toothbrush or water pick or something like that, do it in the shower.
Somebody mentioned that make sure you do it in the shower doesn’t go everywhere, and the other person mentioned lie down, which I had never heard before, but if you have some motor issues or some, you know, real motor problems if you just lie down and then do it, it’s it apparently it’s easier so we’re going to share a bunch more on that but I thought that was fun little tips for those of you out there who are struggling with oral stuff.
Kat Hill:
So, I’m going to quote Mel, lie down and do it.
Melani Dizon:
Exactly. I also heard today that lying down when you’re fighting with somebody, dissolves the fight, because we are meant to be in this mode right, we’re meant to be moving forward when we’re fighting we’re in that sort of state.
And if you are fighting with somebody and you say, lie down and you guys both by down, it’s like not possible to fight. So please, everybody, if you’re fighting this evening, lie down on the floor.
Kat Hill:
I learned so much here!
Mealni Dizon: Yeah, Kevin,?
Kevin Kwok:
Last session, you challenged us a few sessions ago on getting sunlight on our sleep talk. I’ve been doing it every morning and I swear it works, so thank you for that challenge.
Melani Dizon:
Excellent anybody else getting their morning and night sun and and it’s helping them? Good. Awesome.
Yeah, Jackie says we should do a workshop on lying down and fighting or lying down and not fighting, I think it’s a great idea.
Heather Kennedy:
That would be so much fun!
Kat Hill:
I think it’s gonna be really interesting on zoom, that’s all I have to say.
Melani Dizon:
This is going to be great, never before seen we’re going to do it. Thank you everybody for showing up today, I’m so happy to have all of you on this panel. Thank you for joining us and offering your questions and please feel free to email us questions at any time, we’re going to be back next month with more questions and Heather has a fabulous send off wave for all of us.
Heather Kennedy:
May I pull out the whole thing?
Melani Dizon: There we go.
Heather Kennedy: Just this part.
Melani Dizon:
Awesome thank you everybody, bye.
Show Notes
Q: If you have chosen to retire because of your Parkinson’s diagnosis or any other reason, how do you find meaning and purpose in your life?
Retiring from your profession can cause some sadness and loss of identity. These feelings are normal. For some of our panelists, contributing to the wellness of the Parkinson’s community has become the “work” that brings meaning in ways their previous careers did. For others, they choose to use this time to focus on the things that were less attended to when they were working full-time, such as family, friends, and enjoying the moment. Many emphasize the power of mindfulness and keeping a positive attitude about this new phase of life; some have used Kevin Kwok’s strategy of mindfully pivoting to find a new sense of purpose and joy.
Question: Any advice about DBS?
YOPD Council member Heather Kennedy recently had deep brain stimulation (DBS) surgery, and she advises those who have chosen to receive DBS to “be patient.” It has taken Heather approximately four months of trial and error with programming to see the positive results she was hoping for. (She also says that if other women have had DBS and aren’t seeing the results they’d hoped for, they should be sure to talk with their medical care teams about interactions that might be impacting the results. For her, an estrogen patch was interfering with the programming, and as soon as she removed it, she felt like a new person.)
Question: Tips on medications?
Parkinson’s physicians generally recommend starting medications as soon as your Parkinson’s symptoms start to impact your daily life. In retrospect, some of our panelists would have started taking meds sooner than they did, but others became severely ill when first taking medications and therefore explored homeopathic alternatives. As Kat Hill says, “It’s ultimately your decision on how you choose to handle your medications.” Talk to your doctor and consult with them throughout your Parkinson’s journey, but remember that you’re in charge of your care plan.
Question: What do you do when your soul gets tired of fighting and putting in the work to live well?
The YOPD Council members validate this feeling and the reality of depression. Their tips for how to pick yourself back up during these times include:
- Finding an activity that lifts you up when you’re down. For YOPD Council member Kevin Kwok, it’s traveling. For others, it’s calling a friend or getting lost in a good book
- Engage in social situations and call or text people in your support system. Just knowing that you’re not alone can be incredibly helpful
- Help someone else
- Remind yourself that what you’re feeling is impermanent and will pass
- If feeling this way is interfering with your quality of life, be sure and talk to your doctor. There may be medications and/or clinical techniques that can help
- Observe when you’re feeling down. If you pay attention to the times of day when you experience sadness or depression, you can more proactively prepare yourself for those moments. Amy Montemarano says she often feels more depressed in the evening, and in those times, she reads a book to give her brain something else to focus on
- Have pride in what you have accomplished.. Celebrate your victories, big and small
Question: A very important part of living well with Parkinson’s seems to be having people to talk to and a strong support system, but how do you find those people?
Community is such an important part of living well with Parkinson’s, but it can be difficult to know how to meet new people. Our panelists suggest finding connections through:
- Exercise classes
- Support groups (you can start you own if there’s not one in your area!)
- Volunteering with Parkinson’s organizations
- Choosing to be vulnerable enough to ask someone you’ve just met out for coffee
- Local community centers, senior centers, and other gathering places
resources and topics discussed
Camping with Parkinson’s Series
Take Your Parkinson’s for a Spin in the Great Outdoors
Get Connected by Reaching Out to a Ambassador
Medication Management For Motor Symptoms
Dopamine Agonists and Impulse Control Disorders
The Victory Summit® Virtual Event: Mental Health and Wellness
Living Well With Parkinson’s: A Conversation with Brian Grant and Davis Phinney
Helplessness and Hope and Parkinson’s
Want to Be notified for future YOPD Councils?
The YOPD Council meets on the third Thursday of every month, and every session is recorded and shared for all to access. Register for the YOPD Council series here, after which you will be invited to join live and be personally notified when a new webinar recording is posted. Interested in catching up on past YOPD Council webinar recordings? You can find all recordings on a variety of subjects on our YOPD Council Youtube playlist, and don’t forget to subscribe to our channel to be notified when new Youtube content becomes available.
Thanks for Listening!
To share your thoughts:
- Leave a note in the comment section below.
- Ask a question by emailing us here.
- Share this show on Facebook.
To help out the show:
- Leave an honest review on iTunes. Your ratings and reviews really help, and we read each one.
- Subscribe on iTunes.
Listen & Subscribe
Apple Podcasts | Stitcher
*The Third Season of the Parkinson’s Podcast is made possible through generous support in honor of Dr. Margaret Hilgartner.