The author, taking a moment to catch her breath. Photo by Davis Phinney.
Written by Connie Carpenter Phinney
This month, we discussed finding grace together. I was joined for our April meetup by our usual cohort for our monthly care partner meetup: our Executive Director, Polly Dawkins, and two care partner Foundation Ambassadors, Gail Gitin and Pat Donahoo. Gail’s husband lived with Parkinson’s more than 10 years and passed away in 2020. Pat’s wife was diagnosed in 2010.
Ken Hill, a care partner from Oregon and an Ambassador, was new to the panel this month. His wife was diagnosed in 2014. And Parkinson’s has been in our house since 2000, when my husband was just 41.
Next month, our meetup will be on May 7, 2024. We are delighted that Dr. Jori Fleisher will join us. Dr. Fleisher is a movement disorder doctor with experience and research in the care partner space. She was also the lead facilitator for our Care Partner Training in 2023.
Meetup Notes
A PRELIMINARy Observation
At the outset, we acknowledge that the conversations in our meetups don’t fit everyone’s needs. We have listeners who are in their first year of living with a person with Parkinson’s, and others in the end stages. Most of you are spouses, but many are adult children whose parents live with Parkinson’s. There are also some of you who have the important role of being a parent caring for an adult child with Parkinson’s. Some of you are caregiving from far, most of you are in the same zip code and, more likely, the same home.
We also acknowledge how difficult and confounding Parkinson’s can be from person to person. Our advice and the symptoms we discuss could be wildly different than your experience. We do what we can to meet your needs but please know we encourage you to find local support. We also encourage you to meet others with Parkinson’s. Knowing people in your community with shared experience can be a huge help. Thank you for reading or attending. We care about you!
Finding Grace Together
We started the meetup with a brief breathing exercise. I reminded everyone to use their breath to give them a chance to reset and balance emotions, or to down regulate emotions and find a moment of grace.
Grace doesn’t come easily for us as care partners, because we are often frustrated by the actions and behaviors of our person with Parkinson’s. Recently, my care partner stumbled while dismounting his bike and fell on top of me. I landed hard, only breaking my pinkie finger. It could have been worse for both of us, and in a perfect world, it shouldn’t have happened at all–but that’s not the world in which we live.
Gail noted how difficult it is for people with Parkinson’s to have to be always so attentive to their foot placement, their speech, every bite of food they take. She said, “These are things a healthy person doesn’t have to think about.” Reminding ourselves of that gives us more grace to allow our person more room for errors or missteps. Gail reminds us it is the disease, not our person, who is to blame.
We also received an important tip from a listener on practicing gratitude: “I asked my husband to give me one acknowledgement each day for something I’ve done or how I’m showing up! He has done that daily and it has created such a deeper sense of intimacy. I know this being seen for the support I give will become even more important as time goes on.”
Making Space for Connection
We talked a little about changing the direction of our lives because of Parkinson’s and how so much of it is actually good. Ken and his wife took the opportunity to sell their home when their kids moved out. After the sale, they traveled and lived in an Airstream. Ken said letting go of their material goods was liberating and getting out gave them spaciousness to redevelop and grow their relationship so that when they moved back into a more manageable sized home, they felt more able to care of each other.
Communication and Manners
A listener asked a question around communication, specifically about the loss of manners exhibited by their person with Parkinson’s. They wanted to know if others had experienced this as well. Simple niceties like “please” and “thank you” go a long way between humans. We know those words become difficult to say as our person with Parkinson’s progresses, experiences dementia, or simply runs short of energy and capacity. What then? Perhaps leaning into code words or American Sign Language (ASL) will help.
Ken talked about his experiences with his wife and how they have created a system of code words for when they need to table a discussion, knowing that in the heat of a disagreement, they won’t be at their best. He also said they’ve started using ASL to communicate, especially to say thank you. Check out this app to help learn ASL.
It is important that we continue to communicate our desire to maintain and model behavior that doesn’t breed resentment. If your person fails to be polite, remind them how far a simple thank you goes while acknowledging an understanding of how difficult it might be at the time. Facial masking can hide what a person with Parkinson’s is truly feeling. A blank face might be hiding a very happy or grateful reaction; they might not realize how the mask affects other people’s reactions. Acknowledge, communicate, and develop workarounds to keep yourself and your person from becoming resentful and angry.
When dementia is part of the equation, it’s more difficult—but not impossible—to create modes of communication and ways to express gratitude. We are fortunate with Davis’s mom, who lives with severe dementia, that she is able to still express gratitude, but we know others who cannot. This makes the experience more frustrating and less fulfilling for a care partner.
As care partners, we are often asked to step up, but we also must step back at times. This is where grace for ourselves comes in and allows us to revisit hard topics when the timing is right. After I fell and realized I’d really hurt my finger, I asked my person to step away so I didn’t get angry and lash out at him. I knew he didn’t mean to stumble and injure me. We were in a public space and others came to our aid, so we let them help us and didn’t discuss the incident until later. We both promised to take more care next time: for me to remind him to dismount safely, and for me not to turn my back until I know he is on his feet safely.
Forgiveness
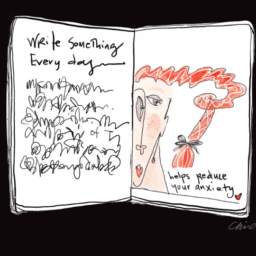
Forgiveness is also an integral part of this equation: Learn from mistakes and move forward. Having or developing a forgiving nature is paramount in this journey. We must utilize tools like meditation, exercise, art, music, simple breathing practices, or other forms of regulating ourselves.
Be proactive and develop a practice well in advance of the hard days to come. You can find resources on our website for developing practical strategies to stay connected and present. Gail said she felt guilty if she engaged with her husband when she felt frustrated. We’ve learned from the social workers who have joined us that guilt is not a very useful emotion, but for some of us, it’s inevitable. Like all emotions, it’s something we must process, work through, and uncover the motives to explore how we can manage better.
Self Care can prevent resentment
Pat talked about revisiting the notion we brought up a few months back regarding the “apple-a-day,” which is the notion that you need something to strive for each day that makes you happy.
What is your “apple”? Is it a bike ride? A walk? Meeting your goal in swimming laps? Making the perfect cupcakes? Is it a good day at the office where you get all your work done? It must be something you can claim for yourself. This is an important part of your mental and emotional health and will ultimately help your person, too.
Pat used the unusual example of cleaning his pool in his backyard in Las Vegas as his “apple.” He says it is cathartic work and that he’s had a tough year with his person, but his pool is very clean. He also gets out to ride when he can and finds that especially important.
Learn more about the apple-a-day philosophy and determine where you are in the caregiving process. Read more about our discussion on this from December 2023.
The Power of Vulnerability
Ken said he has moments where he’s broken down and cried in front of his wife, giving her the opportunity to not only be vulnerable, but to reveal the gravity of his role as her care partner. How many of us do that? How many of us acknowledge how much we dislike the disease while still loving our person?
To be vulnerable and to ask our person for their help in understanding that fact is important work, but very tough. Ken says he was raised to be prepared, but with Parkinson’s you sometimes feel at a loss. He manages with daily meditation and readings. He said he finds reassurance by controlling what he can and recognizing what he cannot control. In this practice, he finds ways to mitigate anger when confronted with tougher issues.
Community Combats isolation
A listener asked what to do about the fact that it’s harder to go out, see friends, go to a movie, or out to dinner. First, we reassured them this is a real challenge; we also acknowledged that getting out and socializing is still very important. Research tells us that isolation is worse for your health than smoking 15 cigarettes a day.
Have your friends and family come to you and be sure to let them know not to overstay. When you invite them, give them a time limit. It’s important to pace yourself and create a manageable schedule so you don’t overdo it. Recruit friends to assist as well if you need help to get your person to a fitness class or doctor’s appointment. Ask them to drive or come and sit with your person, which might give you the precious time to do your own self-care, manage your work, and other necessary tasks.
Another listener asked about later stages in caring for someone with Parkinson’s. Gail said this varies from person to person. One of Gail’s friends had been doing very well, then took a bad fall and suddenly passed away. Gail’s husband first had a slower decline which became very rapid due to Lewy body dementia. He experienced failure of his autonomic nervous system; he struggled with very low blood pressure, and frequent episodes of passing out. Each of us finds different experiences. We acknowledge not being able to answer how life will be or how best to manage.
Build Your Team
The best course of action is to build your team in advance of when you need them. I’ve found that newer friends–those who didn’t know my person before he was diagnosed–have been the most helpful. Many of our friends who knew him when he was healthier are less likely to accept his status and need for help.
The other more helpful group are those with Parkinson’s who rally together and help each other. This is an important step in building the team that will take us into the next phase. Paramount in that is the capacity to ask for advice and help. Don’t forget that as humans, we are hardwired to help each other.
Where do you find like-minded people? We find them at community events or at Rock Steady Boxing and Pedaling for Parkinson’s. We find them because we make ourselves available. If you are struggling to meet others, connect with one of our Foundation Ambassadors.
Links related tO Questions and input from our listeners
During this meetup, we received questions about incontinence and whether it is caused by Parkinson’s. In most cases, we would answer yes, even when your doctor says no: Parkinson’s can wreak havoc on all autonomic nervous system functions.
Betsy offered a game-changer solution: For her person with Parkinson’s, she recommends NorthShore GoSupreme overnight pull on underwear. Others weighed in regarding bathroom issues and Parkinson’s by sharing that they use family restrooms when out and about to assist their person.
A listener asked for resources regarding a family member with a recent young onset Parkinson’s diagnosis; find those resources on our YOPD page.
For more discussion on finding emotional and psychological care, visit the Psychology Today website.
Additionally, check back in with us next month for Mental Health Awareness Month where we will share more resources. On a personal note, I’ve found a resource through my doctor’s office: They recommended a therapist specializing in treating and working with individuals with chronic diseases and/or their care partners. Ask your general practitioner about your options. In my case, their practice included a licensed social worker who helped me find a super specialist. It took about six months to get her lined up, but it’s worth it.
We are here for you
As always, we want to remind you that we are here for you. Please reach us with questions and feedback at blog@dpf.org.
We look forward to seeing you next month. If you aren’t registered to join us live, you can do so at our care partner meetup registration page.
AdDitional Resources
Palliative Care Webinar with Dr. Kluger
Steps to Manage Orthostatic Hypotension
Living with Parkinson’s Monthly Meetup: Tips and Advice for People Living with Parkinson’s