Now is a time for hope for people living with Parkinson’s. Research continues to prove that certain actions and behaviors can help people live well with Parkinson’s TODAY, and there are numerous drugs, surgical procedures, complementary therapies, and other treatments in the works to help treat symptoms and potentially slow or even stop the progression of Parkinson’s. In this webinar recording, movement disorder specialist Michael Okun, MD, shares the latest on emerging therapies for Parkinson’s and what’s coming down the pike for the Parkinson’s community.
Watch the recording below.
Read the transcript below or download it here.
Soania Mathur, MD (Davis Phinney Foundation Board Member, Co-Founder of PD Avengers, and Founder of UnshakeableMD):
Good afternoon, everyone. As Polly mentioned, my name is Soania Mather. I’m a family physician and Parkinson’s patient having been diagnosed now for over 24 years. I have the privilege of serving on the board of directors for the Davis Phinney Foundation and I have the great pleasure of being a moderator today. As you know, Parkinson’s disease, although initially described over 200 years ago, I think 205, it remains a progressive incurable condition, but that doesn’t mean that progress hasn’t been made to increase the treatment options that our medical team can offer us to help manage our symptoms and optimize our quality of life. And there are still other treatments in the development pipeline that may in fact, be disease modifying, changing the course of progression of our disease and to help us navigate what’s new in this area of emerging treatments or therapies is Dr. Michael Okun. Michael’s always so great to have an opportunity to speak with you and today’s topic I think is gonna be particularly interesting and relevant to our, really our entire community, because no matter where you are in your Parkinson’s journey, emerging therapies are always important to know about. I think you and I both say the same thing that knowledge is really power in this disease. So welcome.
Michael Okun, MD (Movement Disorder Specialist, Chair of Neurology, Professor, and Executive Director, Norman Fixel Institute for Neurological Diseases, University of Florida Health College of Medicine):
Yeah, no, thank you. It’s, great to be here. It’s great to be with the Davis Phinney Foundation that does such awesome work for the field and is such an inspiration. I remember sitting next to Davis Phinney at the white house and him turning and saying to me, what is a version of an old Walt Whitman poem make every day, your best day. And so hopefully today, we’ll be able to talk a little bit about that and a lot about, you know, where the hope is for emerging therapies.
Soania Mathur:
That’s great. He is a very inspirational person that’s for sure. I think I’d like to start with a very basic question, but really one that we really should define at the outset and the word therapy. It can be so broad and sometimes confusing for many people. So, what do we mean when we say therapies for Parkinson’s?
Michael Okun:
Yeah. So, when we’re talking about the word, you know, therapy, and there’s a lot of different ways that people will parse that, you know, and there’s Greek derivations and Latin derivations. And the idea is, is that we’re trying to not only provide the potential for what some would call Western medicine, but also the potential for what a lot of Eastern cultures call healing, right? And so, when we bring forward a therapy people forget, they think that a be has to mean something like, well, this is gonna be the cure for this disease, whether it’s a cancer or something that that’s the only thing that a therapy represents, but actual the actual facts are that a therapy can be anything. It can be a drug, it can be a gene therapy, it can be a surgery, it can be an intervention like an exercise or stretching or something that you do a lifestyle change.
It can be how you approach a hospitalization. And so, when we think about tips, when we think about ways that we’re gonna live better today and also think about tomorrow, therapies cross those lines. And so, I always remind people that, you know, we talk about things that can help us today. Those are symptomatic therapies. We’re certainly looking at therapies that might slow disease progression, and then everybody’s interested in the big C could there be cure based, you know, therapies on the horizon in the future. And so, when we think about and have those discussions, whether it’s Parkinson or other diseases, that’s, the context is think more broadly. So, I bring it to the convergence of, I would say Soania, think more broadly.
Soania Mathur:
Great. So, if we Michael take therapy as being really any modality that can be used by patients and their medical team to improve the patient’s quality of life, let’s maybe take exercise and Parkinson’s. It’s something that we all should do Parkinson’s or not, I mean, exercise is healthy for our lungs, our heart, our muscles, our bones, and even our brains. And there are Parkinson’s specific benefits that we also know about, but there’s been some developments in exercise as medicine has there not and can you tell us more about that?
Michael Okun:
Yeah. So, you know, one of the most exciting areas has been this notion that there’s something beyond exercise, that’s just good for our health, right? So, we all know if you read the literature, if you listen to the evening news, if you listen to your doctor or maybe even your spouse or somebody that lives in your house, they all say, well, do exercise. Exercise is good. Well, that’s fine. So why should all of these new guidelines and new recommendations and new review articles and big journals, like Lansing , and Journal of the American Medical Association and New England journal, all, you know, heap praise on exercise for Parkinson’s disease. Well, it’s because lots of the animal models that we’ve seen when we exercise animals, we have little treadmills that we can exercise animals on. And we look at the brain chemicals and the changes there have been some really unique and important changes. The circuitry that have said, Hmm, there’s something going on here that, you know, this may be important. And so, this has been evolving over a number of years, and now we begin to move into this idea where let’s test this in the humans. Okay. And the big animals. Right. And what happens if we do this, will it symptomatically will it improve our symptoms or will it slow disease progression? And these are some very big questions. And certainly, we know that if you offer somebody exercise, their symptoms get better. And if you exercise and you stop exercising, or if you have physical therapy and you stop having physical therapy and you stop exercising in general, we see declines. You know, so we’ve seen this over and over and there’s some literature on this. And the question is, could we now take the next steps Soania and say, what would happen if we gave certain interventions for exercise, could it actually affect the disease progression or maybe even slow disease progression?
And so, there are two studies that have been, you know, examining questions that are starting to take these next roads. We talk about paths, right? So now let’s go down that next path on exercise and see, does it have something beyond symptoms? And so, there’s a study called SparkX in the US, and there’s a study called Park-in-Shape that was done in the Netherlands, by the Dutch. And in particular, folks here should know that there’s a paper out from the SparkX group where they originally had like 130 or over a hundred subjects. And they took a subgroup of those subjects and they gave ’em something called a functional MRI. Okay. And so, this is something where, you know, you put ’em in the MRI machine, you have ’em do something and you look, and you can see what changes and what networks have changed, whether they’re resting and doing nothing, or whether they’re doing the tasks that you ask them to do.
And there were two groups of people in that study. They were randomized into two groups. Okay. And the groups that they saw in that study were groups that got these exercises, mostly with biking, remember the Dutch loved to bike, right? So, we all know that right versus flexibility types of exercises in the other group. And so, there were 25 in one of those groups, 31 in the other group. And it started out with 130 subjects total. And when they looked at what happened to the brain network, Soania, they saw this shift, how the brain networks were talking to each other, how they were connecting to each other. And there was a certain region of the brain. And it’s not important that anybody on the webinar remembers the region, but it’s the front side of a region called the Putamen. I just wanna make sure you know we’re being credible here and I’m giving you credible information. That was thought to be important to stabilizing motor function.
And so, this is beginning to bring forward some evidence to show that the networks for shifting, and then maybe we’re stabilizing some of the things in the brain, it’s early days here, but it’s another step in the right direction. And so, exercise, we’ve always said, it’s like a drug, lots of interesting things happen, like miracle grow on your brain. But, you know, I would say this Park-in-Shape follow up study is really interesting and something that that, that should draw some attention. And we’ll be talking about it on Twitter here probably for a few weeks.
Soania Mathur:
Yeah. That’s amazing. If you think about it as a patient, having that power to actually change the course of your disease, the progression of your disease, potentially through rewiring through something, not always as simple, but as simple as exercise. I mean that’s really amazing. I can see how there might be a prescription pad with specific exercise for you as a patient that will happen in the future. Thank you for that. I think there are some new physiotherapy guidelines for Parkinson’s disease recently released as well. Was there not?
Michael Okun:
Yeah. So, there was a group that that came out, this was an internationally recognized group of physical therapists and what they did Soania is they got together and they said, you know, what do we know? Right. So here’s the frustrating thing if you’re a family member or you’re a person with Parkinson, there are all these studies, they come out and they just come out one after the other. You’re not sure what to read. You’re not sure what’s right. You’re not sure what’s wrong. And then, you know, when you look at physical therapy for Parkinson’s disease and interventions, like exercise and different approaches, it gets very confusing cause there’s so many of them. And so what the group did is they got a group of experts together, dangerous thing, right, but all the experts try to get ’em to agree on something.
And they created, you know, what was a definition for levels of evidence, you know, for the different types of therapies. And so, they did this across all the exercise therapies and they decided to rate in diamonds. So, as you know, some properties are rated in diamonds. So, if you go in a hotel and you see a lot of diamonds, that’s good. If you see a half a diamond or a quarter diamond, you know, you might think about going to a different hotel, right? So, what they did is they went through all these papers, they applied the evidence and they brought forward some recommendations for physical therapists who are treating folks with Parkinson’s about what works and what doesn’t work.
Soania Mathur:
That’s a great way because, you know, there’s such a different level of experience that physiotherapists have with patients depending on whether they have them in their practice. There’s a few questions in the just to go back to the exercise recommendations. Do we know at the moment what those recommendations may be in terms of intensity and in terms of, you know, how frequent we should be exercising?
Michael Okun:
Yeah. So, they made some comments on that. Unfortunately, you know, for the person that’s asking the question and I love by the way everybody telling us all the different areas of the globe that you’re from in the chat and seeing so many folks logged on here, what they were able to tell us was in general, it’s good. Multidisciplinary approaches, very good. Queuing approaches are good and some are better than others. But what they weren’t able to do was focus in on how intense the exercise should be, because there were so few studies in that area and there’s some debate within the field and the debate goes something like this, everybody’s different and if you ask somebody, let’s say to pedal, you know, at the number of rotations, we’re the Davis Phinney Foundation, right, it’s dpf.org today, right? So, if you pedal right along, how many pedals do you get in a minute, right? Your RPMs, your revolutions per minute. Some people can pedal faster. Some people can pedal slower. So, it’s not a one size fits all. So, it’s actually hard. Everybody’s hearts are different. Everybody’s heart rates are somewhat different. Everybody has a different health status. And so, putting you know, firm recommendations has been tricky and then the subtypes of Parkinson’s are different. And so, we have really struggled as a field. And everybody asks that question, you know, from San Antonio, you know, in the middle of the country, all the way to, to Oregon, San Francisco, to New York or Florida across to Australia, everybody says, what’s the intensity. And the answer is, we don’t know. We know that you should sweat. We know you should get your heart rate up. But there’s quite a bit of debate among the experts. And you should know that it’s not a thrilling answer that I give you here, but it is the answer of where we’re at.
Soania Mathur:
Right. Thank you for that. To sort of shift gears a little bit, we also often get questions from the Parkinson’s community, about more advanced treatments that are being developed such as stem cells and gene therapy. What can you tell us about those? What should our people know about those potential treatments?
Michael Okun:
Yeah. So, you know, always when we take talk about emerging therapies, people want an update on that and they deserve an update. And the reason Soania they deserve an update is they’ve been hyped so much, right? Like people say, okay, this is gonna be the cure. You’ve got a dopamine cell problem in Parkinson’s. Let’s put those dopamine cells in, let’s get the show on the road here and let’s fix Parkinson’s. And what we’ve learned is, is that, you know, over multiple transplants with animals and with humans now, with cells that come from embryos and cells, that don’t, we can make lots of cells now, there’s even new techniques to get enough cells out there of people, this has worked for people to be able to get the therapies. But what we found is that it hasn’t been the holy grail, so to speak, for those of you that like a little British humor, there hasn’t been a holy grail here for stem cell therapy. And one of the reasons why is Parkinson’s is complex. It’s been targeted at those motor circuits and some of those motor circuits where there’s the black cells that die. So, the dopamine cells that die. And as we think about the therapy, we can certainly make them more pure. Some supplies will need you to be on drugs, so you don’t reject the cells, but now we’re getting better at that. We’re getting better at the cells turning off so they don’t cause cancers if they grow too fast, but Parkinson’s is such a complex disease that it really has been quite challenging. Now, I would say that one of the emerging things for the field to watch is a group and I wrote this down, cause I knew I would forget it, although it has a name you should remember, it’s called the Stem PD group.
This is a European consortium and collaboration. That’s sort of taking on some of these questions and trying to look at multiple circuits. And then there’s a very a famous researcher who’s in Japan named Takahashi and he’s got some new papers out on stem cells. But, but there are, you know, in terms of the therapies, it didn’t go as far as we would like to see it go. And I think that the scientists in all honesty have had to take a step back and ask that question, why? The other thing just to mention here, since we’re talking about emerging therapies is there’s a great reporter named Laura Biel. And she has a podcast and one of her podcasts is called Bad Batch and it’s her father actually had Parkinson’s and that’s why she made that podcast.
And she’s also done Dr. Death and several other things you’ve seen on TV and other famous podcasts, but listen to the one called Bad Batch, if you’re interested in stem cells, because that one will tell you a lot about how the field has evolved and how it got a little out of control with tourism and took advantage of people and what the hope was and how hope translated into too much hype and how we’ve got to dial it back a little bit and be careful as we’re looking at these therapies. So, there’s still some why questions here on the stem cells. And it’s not clear that this is gonna be the clear path forward that many people thought maybe 15 years ago.
Soania Mathur:
Right. What about gene therapy?
Michael Okun:
So gene therapies are very interesting. And one of the reasons that gene therapies are interesting is that we have a certain number of Parkinson’s cases that are associated with single genetic abnormalities.
Some people call this monogenetic, so 15, 20%, depends on which geneticist you talk to, may have one of these. When you have a gene abnormality, like the LRRK2, or the GBA gene, or one of those, when you have an abnormality like that, then it allows us to say, well, what does that do to the pathway, to the degeneration pathway as it’s churning, what does it do? What’s the function? And can we look at that pathway and try to disrupt it with different drugs and with different genes? And is there a potential like in a therapy like for the Parkin gene, is there a potential to insert in using gene therapy and really get to the heart of some of the dysfunction? And so, there are several trials that have been done, several trials that have been done successfully.
Now, the results may not have reached a level of what some medications and some other therapies like neuromodulation or pump therapies. But the fact that people have been able to do this with relatively good safety so far, that was the big concern was going too fast and then having a pull back and hit the brakes and the field was gonna slow down, gives us some hope that this therapy plus combinations with others could hold some real promise. And you’re gonna see this really focused around those, first those monogenetic types of therapies, but it’s not too farfetched to think it could have some expansion onto others as we understand this technology a little better.
Soania Mathur:
So it could you mean apply to those of us that don’t have any genetic mutations that we know of that have influenced our development of Parkinson’s?
Michael Okun:
That’s right. So, what you’ll see is you’ll see the investigators always start on the well-defined. So, a good experiment starts on a well-defined group of individuals. You figure out how it works and where it works. And then you’re gonna look at off target effects. Sometimes you’ll give something and something good or bad will happen off target. Sometimes you might cure blindness or something and like, okay, well, we’ll take that result and, and bring it over to this field. That happens. And, you know, not infrequently in the serendipity of medicine, but the hope is that whether you have a genetic problem or not, a lot of these pathways are functioning in similar ways, and you’re gonna intervene at similar areas in that pathway or similar steps in the pathway that there may be wider applicability, or it may open the door to understand how to get to the larger group.
The other thing, just to tell people who are listening, we’re talking about emerging therapies, you want to fail a lot. You say, oh my God, I’m gonna turn this guy off. Why is he saying you want fail a lot. You need to fail. Okay. When you do this, you need to fail. And the reason that you need to fail is you learn so much from the failures. You know, you have a hypothesis, you think it’s gonna work this way. You do it, it doesn’t work out. You still need to publish it. We need to teach each other. As we define this, we have to have many more failures to get to the successes. We have to open that funnel up so we’re funding more research in order to get the number of failures to get to the successes that we need. And so, we need to do a lot more research. So don’t be totally bummed out with the failures, cause we need those as well.
Soania Mathur:
Right, I mean, that goes with the saying that there aren’t any failed studies, really because we, like you said, we can learn from every one of them. Something we’re sort of inundated with these days during the pandemic is of course the concept of vaccines and vaccines are also something that our audience probably has heard about in relation to Parkinson’s, the upcoming pandemic in some ways. Can you tell us a little bit about vaccines and where we’re at?
Michael Okun:
Yeah. So, there’s actually a number of different approaches with vaccine therapy. Now you say to yourself, why are we talking about vaccine therapy? We don’t typically talk about, you know, Parkinson’s disease as an infectious disease, like influenza, like COVID 19 or something like that. But it turns out that that’s not the point. The point is, is that, what we can do is we can utilize the immune system, which by the way, your immune system is not completely normal in Parkinson’s disease. I don’t mean to let the cat out of the bag if you all weren’t aware of that, it doesn’t mean that you’re not able to fight off infections about as well as other people, but there are fundamental differences when we look at the immune system of folks who have Parkinson’s and folks that don’t, and that is a very important area of study, particularly for understanding how inflammation and other things affect the brain and affect Parkinson’s and maybe even how Parkinson’s comes to be.
Now having said that we can use the immune system, because what happens when you get an infection, the immune system sees something that it doesn’t like, it recognizes it and then it makes antibodies. So, it goes after it and it breaks it down. Okay. And so that is a fundamental, important quality. And one of the reasons that we can occupy the planet is that we have immune systems. If we couldn’t, we couldn’t live long enough, we certainly wouldn’t be old enough to have evolved to be able to be on a webinar on zoom today. And what we need is we need to think about how could we utilize the body’s response and the immune response to maybe go after some of the bad suspects in Parkinson’s. This has been done in Alzheimer’s before, okay with amyloid therapies. It failed, but there are several other attempts going on in Alzheimer’s disease.
And now there is a series. There are a series of these studies going on across multiple continents, multiple companies, multiple approaches to use the immune system to try to clear off these bad proteins, alpha synuclein, or lewy bodies, try to clean that brain off. And there are multiple techniques to do this. And the big question, Soania is, are you gonna clear it off and it’s gonna be a big, you know, nothing burger? Are you gonna clear it off and people are gonna get betters symptomatically? That’d be good. Are you gonna clear it off and people are actually, it’s gonna actually slow the disease progression? Great. And what will the side effects potentially be? So, it’s exciting. And I should also mention, there are also drugs that can be used against the immune system, like TNF blockers, you see arthritis drugs that are all over the news.
And so that’s another way to get in there on the neuro immune system. And so really, you know, pretty interesting. And then you can also think about combinations of therapies and those who know me know when I talk about emerging therapies, I always say one of the big mistakes that we make is we’re looking, you know, for that one size fits all, that silver bullet, you know, that’s gonna hit it and, and be, you know, the one great thing. But, if we look at our history with HIV, with combination therapies, if we look at our history with cancer, with combinations of chemotherapies, you know, the answer here may not be that we should all be arguing with each other. Maybe we should be uniting and learning how to put these therapies together. Especially as more effective therapies come forward, we’re gonna have the opportunity to do more combinations.
And so maybe gene therapies and drug therapies and other things may come together in a way. And I think we need to be more open minded. And I tell all of the folks that I treat in the clinic when I get to go in and see folks, which is, which is multiple days a week, which is the best part of my job, that medicine is very humbling, right? And you’re a doctor too, Soania, it’s very humbling. Every day I practice medicine, I know a little less, it’s very humbling. And we have to keep an open mind as to what might be either the next therapy or the next combination of therapies.
Soania Mathur:
I think that’s really important. You’re right. I mean, we’ve changed HIV from a death sentence basically into a chronic condition. And that, as you said, came from a combination of different medications or treatments. Drug repurposing, Michael is another term we often hear in relation to emerging therapies and what does this actually mean? Drug repurposing.
Michael Okun:
Yeah. So, if we break this down, it’s really an idea of saying, okay, we’ve got a whole bunch of drugs that have already been FDA approved. We even got a bunch of drugs that are on the shelf that have been tested, didn’t work for their particular disease and they just got put back on the shelf, for a number of reasons, could have been dose, could have been wrong disease, could have been wrong, you know, person. And in fact, I will give you a very good historical example. The HIV drug, you brought up HIV, AZT, that drug was discovered 30 years prior, was designed for cancer treatments, right. And that investigator thought he was a failure because his drug didn’t work that he worked so hard on, but guess what? It came back around and this protease inhibition, this idea of using it against HIV.
We repurposed a drug that was already there and it fit the mechanism once we understood more about the mechanism of the human immunodeficiency virus, we were able to repurpose, and there was something there that we could use. So, in Parkinson, we start to think and have this conversation. And one of the things that we’ve become really good at is taking cells out of people’s brains with different genetic disorders and growing them up in plates, we can do what’s called drug screening to see what these cells will do outside. So, in a test tube, how they’re gonna behave against these drugs. We can do these large-scale screening types of projects. And we can look at things that are on the shelf that might have action against Parkinson’s, or various symptoms of Parkinson’s. And so, the ones that we’ve seen that have come forward that have not been, you know, particularly useful to date, we’ve seen nilotinib, the cancer drug, a couple of studies on that, but there may be other “ib” drugs.
This works in a very specific way on the on the degenerative pathway. So, there’s still some hope for that group of drugs. We’ve seen gout lowering drugs, like inosine, we’ve seen as isradipine, which is a hypertension drug. We see prostate cancer drugs, alpha drugs, iron drugs, things that clear iron out. People have thought maybe that might be useful. I mentioned arthritis, drugs, these TNF alpha drugs, you see ’em all the time for arthritis and people on TV. And so that’s the idea, take a drug that’s already there, try to repurpose it for a different disease, pull it over into Parkinson disease. Maybe their answer is already there and staring in front of us.
Soania Mathur:
And the stats that I’ve heard, and they’re for probably old, but that takes well over a billion dollars and more than a decade to develop a neurological treatment. It’s probably more than that by now, but so does drug repurposing help with that timeline and investment at all?
Michael Okun:
It does. And those statistics are pretty spot on. And may, even as you mentioned be an underestimate, and that may seem, you know, just not acceptable. So, like if I had a disease like Parkinson’s disease, I would say that’s unacceptable, but we haven’t really moved that timeline significantly. And we have to think about ways in which we can do this. And one of the great you know, experiences that we’ve all lived through here has been the operation warp speed to move things faster for the COVID 19 vaccine. And so, Ray Dorsey and I, and Bas Bloem and Todd Sherer, we wrote about the ending Parkinson disease book. And then, we had an op-ed in in the daily beast talking about what we need as an operation warp speed. We need to speed up, you know, because there are people that are suffering now, and we need to do something faster and get more therapies into the pipeline and get our processes moving faster. Our symphonies need to be moving and need to be more synchronized between countries, between health regulatory agencies. We certainly don’t want in any way to put anybody in harm’s way, particularly, you know, because it’s not like if we don’t give you the therapy tomorrow, this could lead to death, but we’ve got to speed up with Parkinson disease’s.
Soania Mathur:
You’re right. It is sometimes when we do see the timelines, but it’s not for lack of the research community trying. And, you know, we have to understand how we can support your work. At the start of the discussion, we sort of talked about what a therapy is and procedures and surgical management are also part of that management of Parkinson’s. I think it was in the forties or fifties that ablative surgery was used where you would actually lesion certain brain tissues to treat the motor symptoms of Parkinson’s, which fell out of favor once levodopa came along. But now we’re hearing about new sorts of ablative procedures, like focused ultrasound. So, can you help us understand what that is and why it’s different from the old school ablative surgery?
Michael Okun:
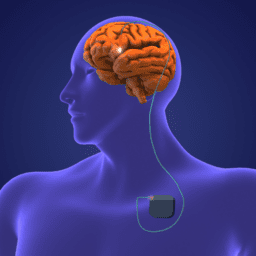
Yeah. So, in about 1958 or so, neurosurgeons actually began to push sound waves into the brain. And so they’ve actually tried this for a number of years, but of course, as you know, even with your computer, sometimes it takes a long time to get the technology to a point where it becomes practical and usable. And so, people have thought about this for a while. It’s a great idea, right? You’re coming from outside the brain, you don’t have to drill a hole, push some sound waves in, you know, focus, those sound waves, and it’ll destroy the brain issue. That sounds maybe a little rough, but it does actually make a hole in the brain. But don’t worry that section of the brain wasn’t working the way it should work anyway. And we know from animal experiments and from humans, that this can provide a great benefit for folks with Parkinson’s disease, particularly when done in the right area.
And so, this has been, you know, sort of a great advance because some people you don’t have to go into the brain, right? So, you don’t have to drill a hole. You don’t have to go through the skull. The problem is it’s still not quite as accurate coming from outside to inside as making a hole, doing micro electrode recording. That’s where you listen to the cells in the brain and figure out exactly where everything is, and once you make a lesion, you can’t take it back and you can’t modulate it and you can’t program it. So, there are fundamental differences. And the other is difficulties with having lesions on both sides of the brain. Historically, we know that that can cause speech and other issues. Now, having said that it can be very effective for tremor, it can be very effective for many of the Parkinson’s symptoms, it’s not a one size fits all, but one of the things that has been very interesting about focused ultrasound is the idea that if you push it into the brain or into other areas, you can actually disrupt some of the traffic. And let me talk about traffic a little bit. And so, you have traffic in your brain. And so, things are going, blood cells are going, medicines are going in and out and you have to protect your brain. And so, there’s this barrier called the blood brain barrier. And we used to think it was pretty impermeable. You know, it was like the force field in Star Wars that was up and it really couldn’t get anything through if the force field was up. And you had to like take that force field down in order to get things through.
We now know that’s probably not true, but one thing that’s been particularly tantalizing about focused ultrasound is using it to break down the blood brain barrier, shoot it in, you know, like Luke Skywalker, you know, put it in there, make a little hole, a little opening, you know, for things. And then you can get drugs and gene therapies and everything across to those privileged areas of the brain. And so, this has been something where people are very interested in, in the development of the technologies. And so, it’s getting paired up with some of these other therapies along the road. And so focused ultrasound isn’t for everyone, but it can be helpful for, you know, some of the symptoms on one side of the body in particular, there’s some studies looking at both sides and then there’s some differences between that and deep brain stimulation, but it’s definitely something you should talk to your medical team about what’s appropriate for you.
Soania Mathur:
And that kind of goes back to the whole combination of therapy. We may see in the future where focused ultrasound is paired up with like the other therapies advanced or medication wise, even to produce results that we need. So, it’s an interesting thing. You talked a little bit about DBS and this technology, although it’s been around for a few years, I think 2002 was approved for use for Parkinson’s. It’s evolving. And so, we are now hearing about adaptive or closed loop, deep brain stimulation. So, what’s exciting about that?
Michael Okun:
Yeah. So there’s a number of us, this is something that those of you that know me know, I do a lot of this for the last couple of decades in our lab, on Tourette’s and Parkinson’s and tremor and things. But there are a lot of investigators who have been interested primarily in how the different regions of the brain talk to each other. Okay. And so that conversation that goes on, so in very simple terms, what we’re talking about is eavesdropping on the conversations, listening to them, trying to decode them, figure out what they’re saying and how that may correlate to your symptoms, whether it’s stiffness, slowness tremor, or even some of your non motor or symptoms, or if you have a different disease like Tourette, maybe it’s a tick. Like what, where in the brain do ticks come from, right? Where in the brain does a tremor come from?
What is that abnormal conversation? And then once we can monitor it, so when we put the deep brain stimulation lead in now, there’s been a lot of experiments in the laboratory, but now many of the systems can listen to the cells that as they’re talking, give you a signal and we call that a local field potential. It’s a squiggle. That’s all it is. It’s a squiggle on a screen, looks like an EKG, but it’s the squiggle of your brain cells talking. And we can use that squiggle to see how the symphony is playing, how synchronized it is, sometimes even in multiple regions of the brain. And we can program it in order to respond to the signal that it sees to help your specific symptom. It’s not clear at this point, whether that is useful in terms of being shown this in a clinical trial, whether it’s gonna reduce side effects or it’s gonna help people whether it’s gonna reduce battery life and make it a better procedure.
But there are a lot of reasons why with specific symptom profiles, we think this may have some benefits for folks with Parkinson’s, so early days here, but now seeing it move from the laboratory into humans and what we have now is a device that’s out there where we can actually look at it, but the closed loop portion, that means we turn it on in that mode. Those of us that are doing it are doing this in the context of research only studies. And so, we’ll see if we see that, I would predict you’re gonna see that at least in a subset of people coming forward.
Soania Mathur:
That’s amazing. So, it’s not just one way anymore. We’re kind of developing that two-way communication between the DBS, the stimulator and your brain really.
Michael Okun:
Yeah, that’s exactly right. And beginning to appreciate that and also now we’re getting a look at things that are going on in the human brain. You know, we get to peek in there and see, a number of us have done this on the lab for many years, but now in the human, we can peek in there and see. And so, for example, those who are in my practice know one of the favorite things I like to do for two decades is, if you, if you wake on up in the middle of the night, it’s very common, here’s a good pearl for you, it’s very common with Parkinson to wake up at two or three o’clock in the morning and you can’t get back to sleep and you sit around and you, and it’s very bad and it disrupts your next day.
And most of the time, it’s because of a beta oscillation in your brain, and the beta oscillation goes up and you just need to simply, re-dose your sinemet, your madopar, your dopamine replacement therapy. And then 20, 30 minutes later, your brain will settle down that symphony settles down and you’ll go back to sleep. But now, we can actually see what we thought we’ve been doing with these reemergence symptoms. We can see the synchrony change at night because we’ve got some eyes on you. And so, what’s really cool and we we’ve done this in epilepsy even a little bit more than we have in movement disorders is the ability to monitor. And so, people with seizures, for example, now we can actually see things we couldn’t see before. Like some people, for whatever reason, everybody’s different, right. You know that in Parkinson’s, same in seizure, for whatever reason, some people will seize at 9:00 AM, you know, or they’ll get more activity around 9:00 AM, but not a lot of activity on their brain later in the afternoon. So, guess what, when do you wanna, you know, double up on your medications, your seizure medications, and so knowing the circadian patterns, and so it does unlock some things that are gonna help us I think, to understand management better, even if in 20, 30, 40 years, the therapy looks very different. It’s teaching us a lot.
Soania Mathur:
And does this circadian rhythm or the sort of symphony of brainwaves you’re talking about, have anything to do about light therapy that we hear about? Or sort of separate things.
Michael Okun:
So we don’t know, but actually if light therapy works, okay, so there’s a couple of different forms of light therapy and many of you actually don’t realize it, but you have already done light therapy because if you go out in the sun or you live in different regions of the world that are darker, you know, at certain times there are higher rates of depression, higher rates of mood issues, a lot of these non-motor issues that come out in Parkinson’s, right? So, if you live in Iceland, it’s different than living in New York City. Okay? The pattern is different of light. That affects your brain. So that, Soania is actually going to affect how your brain is oscillating. And so, we know about this more in animals than we do in humans, but we’re gonna begin to get this information in humans and see that.
So there have been a couple of studies of light therapy. They’re pretty interesting, not a large, you know, amount of change, you know, but some interesting things that had been seen, there’s a study that came out of out of Harvard out of Mass General that was nice, that taught us a lot of things about light therapy. But then there’s also this near infrared therapy. And people have been putting this, you know, like near infrared rays that go into your nostril into your nose. And people are selling these devices. There’s a couple of different companies that are, you know, marketing them. And the real question is do they do anything? And so there actually are a number of different studies. There’s a Parkinson Foundation funded study at the University of Florida, where I’m at, where they’re actually looking, trying to look at those outcomes and see if this is worth pursuing.
And so, there are some interesting studies now in the literature. And you know, like I said, at the beginning, you know, every day I practice medicine, I know a little less, and I tell you we have all these conversations on Twitter and people bring up like, what, you know, 20 years ago, I would’ve said, oh, you know, that’s probably a little crazy. Now I actually pause. And I think about, you know, okay, let’s just consider this for a minute, because I think we probably have been a little too dismissive of things. And it’s really up to us to see if there’s anything to it. And of course we don’t want people to get taken advantage of with certain types of therapies or get sold a lot of things that aren’t gonna work. But I do think that it’s wrong for us to dismiss these things and this light therapy, I think, needs to be tested and so we’ll have some data here soon from here and there’s data and other studies that are going on in different diseases as well. And so to be determined.
Soania Mathur:
We’ll have to wait and see. You mentioned depression and that is obviously a non-motor symptom of Parkinson’s that really can people’s quality of life in all dimensions. So, there were some questions about ketamine and PCP treatments for depression that people have heard about. What are those treatments and what should we know about them?
Michael Okun:
Yeah. So this is really just absolutely fascinating, Soania. I mean, this is really cool stuff. And you know, who woulda thunk it, right? You know, like, but again, you have to have an open mind to these things. And so, there is this drug called ketamine, and we know that people can use this, anesthesiologists can use this, you know, for sedation, but there are also two effects, at least two effects that are of interest to people that are watching, who have Parkinson’s or know somebody with Parkinson’s. One is a potential antidepressant effect. And we all know that depression is the largest unmet hurdle in Parkinson’s, at least some people believe it is. I believe it probably is and ketamine can also potentially suppress dyskinesia. And there are studies. So, if you go to clinical trials.gov, which is where all the clinical trials are registered, and I probably should have said that upfront, we’re talking about emerging therapies.
So, people that are doing these studies usually register them with this national government registry. It does not mean they’re legitimate. Okay. So, there are, you know, studies that are maybe on the fringe of various therapies like stem cells and other things that are still registered. You can’t stop people from registering, but at least it’s an area to start your discussions. Now, when it comes to ketamine, we’re thinking about it for depression. We’re thinking about it for dyskinesia. What does it do? Well, we’re not sure in Parkinson’s, but we think it has something to do with affecting the way that the brain cells burst, this burst firing of brain cells, and there’s a receptor called NMDAR. And that receptor seems to be important to this response and a chemical called serotonin that is super important to depression.
And so, we think from the depression, we think when we give this, we can reduce people who have suicidal ideation and relieve depression. And the question is how do you do this acutely? How do you do this chronically, how would it be applied? Now it has been abused. People have put it into all sorts of street drugs, you know sniffed it, done all sorts of stuff. Just, you can imagine that. And so, we obviously, we don’t recommend anybody go down that road at this point in time, just wait a little bit more until we get some data, cause this can be an unsafe therapy to try to do on your own. And if you try to get this therapy on the street, I got news for you. It turns out a lot of times it’s laced with things that you don’t want.
So I wanna throw out a little caution here on that. For the dyskinesia story, there’s a chemical like a miracle grow in the brain called BDNF and it affects that sort of chemical and that, you know, seems to be kind of the miracle grow. And we think it’s affecting some signaling on something called TOR1. So TOR1 signaling and in some way it seems to be suppressing these extra movements from dopamine. So, stay tuned, you know, open mind. I don’t think we had an open enough mind to ketamine and we’re opening our mind. Now the real mind blower here has been PCP, right? So, you see all these movies, maybe some of you are in school and you see the guy on PCP breaking through handcuffs. It was developed as an IV anesthetic. And you’re thinking this is recreational drug use.
You know, like why would I be interested in this? Well, it turns out that these drugs called hallucinogens, if you give them in micro doses, tiny little dosages, so there’s LSD, which comes from the ergot, so, it’s part of that wheat, you know, the chaff in the wheat, that area, POT, that comes from cactus and has mescaline in it, psilocybin, you’ve heard on the news from mushrooms. And then of course, PCP, which we use, used to use as anesthetics. We don’t use it anymore. If you give little teeny tiny doses, particularly psilocybin, with people who have PTSD and very severe depression. It seems to reset and maybe even rewire some of those brain circuits that are important. Now you have to do this with a guide, you know? So, somebody’s there with you and guiding you through the experience that’s done in the form of clinical trials. Okay. And for research. And they’re just starting to look at this in Parkinson’s and other diseases, but it’s been very powerful in PTSD. Do we know what it does? Not totally, but it seems to have effects Soania, on the brain, on the spinal cord and on that drug again where ketamine works on serotonin. And so, a lot to learn here, but could be very interesting. Cause think about these little tiny dosages might actually change your brain network and it might actually rewire. And that’s the question, if it rewires, how long does it rewire? Could this be a very powerful treatment? So, people dismissed it, but it ain’t gone, guys. It’s gonna make its comeback. As we learn more about what it’s actually doing. I think it’s a very interesting drug.
Soania Mathur:
Very interesting. And speaking of recreational drugs, there’s lots of questions in the chat about cannabis and Parkinson’s and is there anything new that we know?
Michael Okun:
Yeah. So, there are a number of studies that are ongoing. So again, if you look at clinicaltrials.gov, you’re gonna see ’em all over the world. Everything from Israeli studies to European studies, to studies in the US, little harder to study cannabis with THC. So, we talk about CBD without and with and without lots of different formulations. So, it’s not a one size fits all. And guess what, when you read the studies, you’re gonna have to understand what the formulation was and how it was given. And so just because it fails doesn’t mean that it fails. So, there’s a lot of work to be done because one bit of cannabis is not the same as another and one form and how you get it is not the same. Never get it from gas station I always say. Never get it off the street, cause it’s often laced, you know, with things that you don’t want in it.
And one of the things that we have said, and back in 2015, we wrote a book called the 10 Breakthrough Therapies. Now obviously we can look back and see where some of these things ended up when we talked about them seven years ago. But, I was highly criticized for talking about cannabis, you know, at that time. So, you think about you know, like where things are and classifying it as is one that might come forward. And we thought about it as could it help with anxiety, sleep and pain, anxiety, sleep, and pain. And now there’s been a number of different studies in the literature that are showing exactly that effect, not as much on dyskinesia and motor symptoms, a lot of the non-motor symptoms, but anecdotally, what we’ve been seeing in the clinic as neurologists, psychiatrist, general docs, what we’ve been seeing is anxiety, sleep and pain.
And then I just read this morning on the Michael J. Fox Foundation website that they had a a study that Rachel Dolhun tweeted out this morning, showing that the patients, you know, in their survey showed those three symptoms again. And so, I think we’re starting to see some convergence, I’d like to see more data, I’d like to see how it works. And then one other thing just to tell you is, is look at, you know, you can get formulations with and without THC okay, the THC is sort of the psychedelics and remember that this can affect your driving and particularly with the THC amounts that are in it, very important to talk to your docs and your multidisciplinary teams, because if you’re driving, accidents go up by 50%, if you’re driving, that can be a danger, but some people with bad anxiety, bad sleep, bad pain have just done so well for us, that it has definitely stuck around.
Soania Mathur:
That’s great. The other one question that we’re hearing a lot of in the chat is cognition. Are there, is there anything new or emerging when it comes to cognition?
Michael Okun:
Yeah, so, you know, when we think about, you know, what’s going on in the brain, you know, and could we, you know, be harnessing different receptors, different areas. People have tried to stimulate different areas of the brain, even with deep brain stimulation. So, there’s some, you know, early work in that area, certainly the drugs that, the targeted drugs that we’ve gone after, like cholinesterase inhibitors, Exelon, Aricept, Namenda, many of you may know these by different names, depending on which country or which zip code you’re in. Haven’t had a huge, what we call effect size. So even if they improve things, they just don’t improve things enough. And I think some of the exciting things have been some of the antibody therapies. You saw the very controversial approval of the Alzheimer’s drug, but there are others coming down that pipeline.
The interesting thing about some of those drugs that are coming down the pipeline is they have a very different mechanism of action. So that’s good. Right? And, I think we need to be looking in different circuits. We need to look beyond the dopaminergic circuits. And we have seen, even with those drugs, some of the drugs that were approved for Alzheimer’s work a little better in a lot of the patients in Parkinson’s, some of the cholinesterase inhibitors than they did actually in Alzheimer’s, at least clinically. And so, I think we are actually gonna benefit as a field from the dementia field out there are in front of us and repurposing their drugs across with us. And so, now I think it’s really a question of going after some of the different receptors, some of the different areas and thinking out of the box for therapies.
Now, one of the things I like to do is very simple. I like to have people get an audio book and listen to that audio book with somebody that they like, and then stop at the end of the chapter and then explain the chapter back. So almost like a teach back and that’s called stories memory and neuropsychological, and you can try to strengthen your stories memory, which is one of the functional things that you need to do in your life. And so, it is important to use your mind, do different things. That’s also another way to train your mind they say the mind is a muscle. So, remember you do that and then watch out for all these therapies on TV that say, they’re gonna increase your cognition. Some actually may make you worse, like coconut oil.
Soania Mathur
That actually brings up my sort of, I guess, last question as we draw to a close. I think that as people living with Parkinson’s, we have to be really careful consumers of information. A real problem with how our community often, finds out about emerging therapies or medications being studied, it isn’t in this really, you know, great forum, but it’s the hype that can be generated when the news hits the mainstream media first. And the context and actual benefit to patients is often overblown. That misguided hype that is generated can really be actually quite harmful. And so, what should people keep in mind when they read or hear about new or emerging therapies for Parkinson’s? How can we be better or more informed consumers of that information?
Michael Okun:
Yeah. So, one of the things that we always tell people is, you know, it is very important to stay up on things. Okay. And so, if your doctor, your healthcare professional says, don’t read anything, I’ll tell you all the answers. I’m not thrilled with that advice. So I think people should, I think you should try to read, and I think you should ask questions and I think you should have an open mind and try to come at this, you know, come to the table with some humility, you know, and understanding how complex it is, but also come to the table with the realization that there are things that you can do that can make you worse. And those of us that have been in the field long enough know that, you know, they say, well, I have Parkinson. So, what could be worse than this?
Trust me, trust me. I have seen people, you know, make things worse. And so sometimes we mix medicines together. Sometimes we inadvertently do things with supplements. Sometimes we lose our entire, you know, amount of life savings on a therapy that we get sold. And so, I want people to go into this with eyes wide open, always ask questions, stay informed, but look for a couple of the tips that we always say is if it is not something that’s approved by the FDA, for your indication, you need to ask a lot more questions, need to ask for, is it a study or not? Is it registered on clinical trials.gov, one checkbox. Good. Does that mean it’s legitimate? No. Then give me the what’s called the protocol for the study and the informed consent and let me bring it to my team of people.
Okay. Would you get into, you know, a car that wasn’t tested, you know, a brand new Elon Musk, best Tesla ever, but nobody had ever driven it before and let it go onto the mode where it drives itself or would you want have that car tested or crash tested a little bit, give it to some people that you trust, who needs to be in the room, and let them look at it. Don’t rush into this. So, I always say slow down. Okay. The first thing you do when you’re looking at an emerging big therapy, slow down, ask yourself if it’s so good, why hasn’t everybody else done it? Get the informed consent, make sure it’s on clinical trials.gov and the protocol, and have an open mind. If you show it to people that you trust to tell you that this is lousy science, or this might hurt you and get a couple of opinions and people say to me, oh, well it’s only $50,000.
Only a $100,000, only $200,000, or I should do this, or I should try that because my friend did this, or my friend did that, don’t do that. Just read, stay informed, ask lots of questions, look for it on clinical trials.gov, get the consent, get the protocol, ask who needs to be in the room and just go into it with the sense of an open mind and know that if you do something that you know, that we don’t recommend, we shouldn’t yell at you. We shouldn’t kick you out of our practices. We should be your cabinet advisors. And that’s what I tell the people I take care of. I’m never gonna do that. Just tell me what you did and let’s work our way through it. We’ll try our best to give you the best advice we can. But at the end of the day, you’ve gotta make the decisions, you know, for yourself. And we just want to prepare you, put that information in your hands so you can make the best decision for your life. And that’s really the core and just slow down. Don’t try to take it so fast.
Soania Mathur:
That’s great advice. And the hour’s just flown by. I can’t believe it, but thank you all kindly for joining us today. I hope you found the discussion helpful and educational. I know I did. And thank you Dr. Okun for your time and expertise as usual. And remember everyone, we may not have a choice in our diagnosis with this disease, but how we face the challenges that it brings is really ours to define. So, I always say to choose to optimize your quality of life, educate yourself, empower yourself. And as Davis says, celebrate your daily victories. And from me until next time, be well and stay safe.
To download the audio, click here.
Show Notes
The term “therapy” can refer to any method or modality that can be used to improve your quality of life. While there are many new and exciting treatments and methods being research and explored, there are a number of false advertisements in this area as well. This can make it difficult to tell fact from fiction. Dr. Okun suggests people with Parkinson’s approach everything you hear with an open mind, ask lots of questions, and share the information with someone you trust to get an outsider’s perspective.
Read on for the latest on a number of different emerging therapies for Parkinson’s.
EXERCISE
- Exercise has been found to reduce Parkinson’s symptoms, and a lack of exercise can make symptoms worse
- There have been many animal studies that show important changes in the brain circuitry from exercise, and studies are now moving to testing these hypotheses on humans
- Two studies in particular, the SparkX and the Park-in-Shape studies, have shown increased activity in the front side of the putamen (a brain region important in stabilizing motor function) with exercise. For a summary of the studies, click here
- While there are no definitive studies on the best exercise intensity and duration for people with Parkinson’s, it has been shown that multi-disciplinary (meaning different forms) exercise is beneficial, as is exercising with enough intensity that you sweat
Stem Cell Therapy
- While stem cell therapy has been hyped by media as being the possible “holy grail” of emerging therapies, it has not produced as many positive results as scientists were hoping, so now they are trying to figure out why
- If you’re interested in learning more on this topic, check out the podcast “Bad Batch,” research done by Takashaki, and The Stem PD Group
Gene Therapy
- Researchers are currently exploring the possibilities of gene therapy for people with Parkinson’s who have a single genetic abnormality (about 15-20% of people with Parkinson’s)
- In time, researchers hope to see if gene therapy has possibilities of treating people with Parkinson’s who don’t have this single gene abnormality
Vaccines
- There is a series of studies investigating the possibility of manipulating the body’s immune system to “clean off” certain proteins in the brain (alpha-synuclein and Lewy bodies) created by Parkinson’s
Focused Ultrasound
- Focused ultrasound involves pushing soundwaves into localized areas of the brain to burn sections of the brain that are not working properly
- This has been very helpful for some people and is a non-invasive procedure (meaning surgeons can do it from outside the skull)
- Focused ultrasound is able to interrupt the blood brain barrier (the body’s natural defense to keep harmful materials out of the brain), so researchers are exploring the possible use of focused ultrasound with other therapies in the future to get drugs, gene therapy, and other potentially helpful treatments to the brain
Adaptive/closed-loop deep brain stimulation
- There are now deep brain stimulation devices that can track brain activity and correspondingly adjust the impulses sent out by the device in response to this tracked activity
Light therapy
- Sunlight can affect your brain and how your brain is oscillating. There is a study out of Harvard and Mass General that shows this effect
- There has also been an interest lately in the use of infrared therapy, which researchers are currently studying. A study from the University of Florida shows some possible benefits of this therapy
Ketamine and PCP
- Ketamine has been shown to have an antidepressant effect and can potentially suppress dyskinesia
- Micro doses of PCP for people with severe depression and PTSD have been shown to sometimes “reset the brain circuits.” Studies for the use of this is Parkinson’s are still in their infancy
Cannabis
- Cannabis has many variations, so there are numerous ongoing studies about its possibilities as a Parkinson’s therapy
- Multiple studies have showed that cannabis can help with anxiety, sleep, and pain
- It’s important to note that formulations of cannabis with THC can affect your driving, so use with caution
Therapies for Cognition
- There is early work being done attempting to stimulate certain areas of the brain to improve cognition
- There have been some small sample size research studies investigating the effects of certain medications on cognition, but larger studies need to be done
- Scientists are looking at repurposing certain drugs used for Alzheimer’s to be effective for improving cognition in people with Parkinson’s
additional resources
- Cannabis and Parkinson’s
- Clinicaltrials.gov
- Sunlight and Parkinson’s
- Follow Michael Okun on Twitter
- Exercise and Parkinson’s
- Living with Parkinson’s Disease and Parkinson’s Treatment: 10 Secrets to a Happier Life, By Michael Okun
- Ending Parkinson’s Disease, By Michael Okun
- How to Exercise to Live Better with Parkinson’s with Jay Alberts
Explore more
For numerous additional resources on specific topics including but not limited to exercise, complementary therapies, deep brain stimulation, and more, visit our Topic Page Hub.
more about the speaker

Dr. Michael Okun received his medical degree with honors from the University of Florida. He was fellowship-trained by Mahlon DeLong, Jerrold Vitek, and Ray Watts at Emory University in Atlanta, Georgia, before founding the movement disorders program at the University of Florida. He is currently Chair of Neurology, Professor, and Executive Director of the Norman Fixel Institute for Neurological Diseases at the University of Florida Health College of Medicine. He is a co-author of Ending Parkinson’s, Living with Parkinson’s Disease and Parkinson’s Treatment: 10 Secrets to a Happier Life.
Live Well Today Webinar Series Presenting Partners*
 *While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.
*While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.