In this month’s Living With Parkinson’s Meetup, we hosted the first of two sessions on fear and shame. Panel members discussed fears they had when they were diagnosed that didn’t come to pass, fears they had when they were diagnosed that did come to pass, and fears they currently have that they’re working through. They also offered some thoughts about how to navigate fears.
Watch the video recording and see other resources below. See you next month on June 15, 2023, at 1 pm MDT.
Not yet registered for the monthly meetups? You can do that here.
You can download a transcript of this month’s meetup here.
Note: This is not a flawless, word-for-word transcript, but it’s close.
Show Notes
Early Fears and Fears around the Time of Diagnosis
The panelists’ early fears around Parkinson’s can be grouped into the following overlapping categories:
Family
Multiple panelists feared the effect their diagnosis would have on their ability to maintain relationships with friends and partners, as well as how their diagnosis would affect their children.
Some panelists noted that they did experience significant changes to friendships and partnerships, and some had lost friends or experienced divorce after their diagnosis. Still, while Parkinson’s had influenced many of their existing relationships in ways they feared, Parkinson’s also sparked many new relationships for them.
Some people on the panel and in the chat shared their fear of outliving a spouse or partner and being alone. Brian gave two actions that have helped him navigate the experience of losing his wife and care partner: 1) having things he loves to do and 2) helping to make a difference for others outside of his immediate family.
Work, Career, and social connections
Panel members discussed a range of fears related to their careers and social connections. Some expressed fear that Parkinson’s would cause them to be alone, marginalized, and left out of opportunities to connect with others because of Parkinson’s. They also discussed fears about becoming out of control and losing the ability to do what they loved to do with their friends and family, especially travel.
Robynn said that one trick she employs when preparing to travel is to always assume there will be a third party (Parkinson’s) joining her and her boyfriend on the trip. Planning trips around the needs of all three parties has made travel more manageable.
Robynn also said that because of concerns related to the stigma associated with Parkinson’s, she kept her diagnosis private for a long time. When she learned that people in her life figured it out before she told them, she realized that nothing bad happened, and it had been a much bigger concern for her than it was for them. This called to mind the overlap of fear and shame, which we’ll talk about during next month’s meetup.
Another fear discussed was the fear of missing out on future plans, like an activity-filled retirement, because Parkinson’s might make the dreams they once had impossible. Kat mentioned that she had these fears because of some of the difficulties she experienced while working full-time with Parkinson’s. However, once she began to work less, she was able to rest and find better sleep patterns. This has helped her meet some of her hopes for retirement.
Parkinson’s Symptoms and Progression
One of the most common fears panel members discussed was fear and anxiety around the unknowns of Parkinson’s. While some of these unknowns relate to work, social life, partnership, and raising a family, they also talked about fears related to their uncertainty around how fast their Parkinson’s will progress.
Kevin said he tries to incorporate lessons picked up from those who’ve been living with Parkinson’s longer than he has. One of the lessons he’s learned is that Parkinson’s will progress and that that can be OK. There are still opportunities to grow and learn. For example, he has recently taken up skiing and LOVES it!
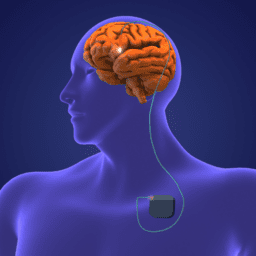
Doug said that although his Parkinson’s was progressing at what seemed pretty quickly, and he started experiencing troublesome dyskinesia that caused him to become more isolated, he found significant relief from DBS, and that has allowed him to reengage in a variety of meaningful ways.
Navigating today’s fears
Today, some of the panelists are dealing with fears around speech, falling, recovering from an injury or fall, freezing, balance, and isolation. They noted that these are likely fears that will remain in the background, hopefully, the longer they live with Parkinson’s. But, they also talked about ways they’re dealing with them so they don’t take over their lives.
Grief and Loss
Panel members mentioned grief and loss multiple times. They talked about missing out on opportunities to have a family or advance in their career. These feelings brought some to tears, and it really drove home how many aspects of life Parkinson’s effects and how many of them go unnoticed by others. We have offered some examples of how to navigate grief and loss through palliative care, poetry, and our resources about mental health.
The Common thread: the power of the Parkinson’s Community
One topic that persisted throughout much of this month’s meetup was the idea that maintaining a connection to a community of people with Parkinson’s can help you navigate and manage fear. Additionally, being engaged with a Parkinson’s community can expose you to the diversity of experiences people with Parkinson’s have. While this may not help with anxiety about unknowns, it can help soften fears related to the specific symptoms or side effects of treatments by helping you learn from others. Connecting with a community and making new friends can also help you mitigate apathy and find new things you can do to live well. At the broadest level, connecting with the Parkinson’s community helps you see that you are not alone, and we all need to feel some of that.
Further Reading: Links Shared during the Meetup
Living with Parkinson’s and Deep Brain Stimulation (0-3 years)
Living with Parkinson’s and Deep Brain Stimulation (6+ years)
Davis Phinney Foundation Ambassadors
Kat’s Book Being Well with Chronic Illness
Carol Clupny’s Moment of Victory
Podcast: Traveling with Parkinson’s
Blog Post: Traveling with Parkinson’s
Exercise, Freezing of Gait, and Postural Instability
WANT MORE PRACTICAL Resources LIKE THIS?
You can learn much more about living well with Parkinson’s today through our Every Victory Counts® suite of resources. Each manual is packed with up-to-date information about everything Parkinson’s. Click the link below to order your manual(s).
Thank you to our 2023 Peak Partners, Amneal and Kyowa Kirin, and our Every Victory Counts Gold Sponsor, AbbVie Grants, for their ongoing support of these must-have manuals. Additionally, we’d like to thank Barbara and Dale Ankenman, Abby and Ken Dawkins, Bonnie Gibbons, Gail Gitin in loving memory of Gene Gitin, Irwin Narter, and Lorraine and J Wilson for their generous donations that allow us to make these resources available and free to all.