Written by Marty Acevedo, RD
I grew up in the South, where my favorite meals included fried chicken or pulled pork, green beans cooked all day with a bit of fatback for seasoning, banana pudding and pecan pie, and lots of sweet tea. As I learned more about nutrition in general in pursuit of my degree and, ultimately, my career as a registered dietitian, my personal “diet” began to change. A move to California solidified my commitment to a healthier lifestyle.
My diagnosis with young onset Parkinson’s came at 44; like many people, I felt several symptoms preceding this diagnosis for at least a decade. I’m convinced that the internal tremor present for as long as I could remember played a role in maintaining a healthy weight. Perhaps, my “diet,” based upon the then-popular Food Pyramid, along with my commitment to exercise, delayed the onset of symptoms.
Like most of us, my knowledge of Parkinson’s was limited when I learned of my diagnosis in 2004. My education had provided limited insight into nutrition for Parkinson’s, other than how protein intake might require modification around the timing of carbidopa/levodopa dosing.
Naturally, my science and medical background led me to research every aspect of Parkinson’s, including nutrition.
I quickly concluded that a lifestyle that included intake of fresh fruits and vegetables, lean meats and more fish, whole grains, lower-fat dairy products, and moderate intake of sweets and alcohol would continue to serve me well. While my research delved into other “diets,” such as keto, paleo, gluten-free, vegan, intermittent fasting, and other meal plans, I knew that a Mediterranean, plant-based diet made the most sense for me. After all, this was not a significant change for me and is consistent with my lifelong mantra that there are no “bad” foods and that we should practice moderation in all things, including our nutritional intake.
I’ve always felt that we should get our nutrients from food, not from a pill or supplements. While supplements are warranted when deficiencies are identified, they are usually not necessary for most of us. Like in Parkinson’s, there is much that we do not know and fully understand about nutrition. There may be beneficial substances in food that we’ve yet to identify. Those nutrients that we have identified work synergistically to provide us with all 197 the tools necessary for our bodies to work and thrive. For example, the Mediterranean diet provides vitamins, minerals, fiber, carbs, protein, fat, and other nutrients necessary for each of us.

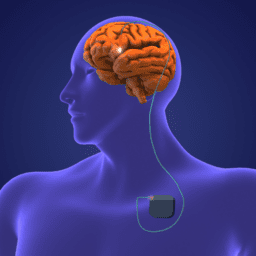
I’m fortunate to have benefited from exceptional care, including appropriate medication and deep brain stimulation (DBS) five years ago. While DBS gave me my life back, the procedure also resulted in unexpected weight gain, even though my diet did not change and I had begun to exercise more than I ever had. Likely, my resting energy expenditure diminished once that internal tremor and my dyskinesia were no longer present. But because I value the benefits of better managing my symptoms through DBS, I can certainly live with a higher number on that scale.
My outlook is that we are best served by adopting a healthy lifestyle rather than following a specific “diet” or worrying about our weight. To me, this means healthy, balanced meals that provide appropriate nutrients, identification of problematic foods (for example, I am lactose intolerant, so adjust my food choices accordingly), adequate intake of water and other liquids, and daily exercise.
While there is no particular “diet” universally recommended for Parkinson’s, the Mediterranean diet and lifestyle include foods that act as antioxidants and are phytochemicals.
Foods with these properties may well have a positive impact on the progression of Parkinson’s, along with a potential neuroprotective effect. Further, adopting the lifestyle aspect of this way of eating—more relaxed, with fewer stressors, a renewed sense of acceptance and appreciation for life in general, and regular exercise—has enhanced and improved my journey in ways I never thought possible.
Living well with Parkinson’s is truly a journey, and that journey is different for each of us. I’m beginning my seventeenth year of living well with Parkinson’s and look forward to what’s yet to come. I believe that the lifestyle I’ve chosen, along with a strong support team of clinicians, family, and friends and an equally strong sense of purpose in my life will allow me to continue to live my life well with Parkinson’s.
About Marty Acevedo
Marty Acevedo was diagnosed with essential tremor in 2004 and with Parkinson’s in 2010. She says that she experienced gait disturbance, dystonia, and REM sleep behavior disorder ten years before her diagnosis. After her progression through the grieving process, Marty decided that her diagnosis would not define her life. Marty felt called to help others who share this journey and quickly became involved with the Parkinson’s Association of San Diego. Serving as secretary on the board of directors, she targeted her knowledge and passion towards educating others living with Parkinson’s, encouraging exercise and socialization, and helping others to find their best life.
Marty is most proud of her involvement in developing and implementing an integrated, medically evidence-based program for people with Parkinson’s at a local wellness center.
Marty is an avid traveler with her husband and their travel van, having covered 35 states and multiple national parks. Exercise, enjoying the ocean and beach, maintaining and cultivating new friendships, learning new things, and sharing her positive outlook are all vital to her daily life.
Learn more about nutrition and parkinson’s
Two of the most common questions we’re asked are these: “What should I know about Parkinson’s nutrition and hydration, and what should I eat now that I have Parkinson’s?” The answer is that there is no one answer. Just as each person with Parkinson’s experiences different symptoms, each person reacts differently to different types of food. The key is knowing that the foods you eat affect how you feel, and this knowledge can be a decisive first step in finding more ways to live well. In this collection of resources, we look at some of the latest research on eating well for Parkinson’s, advice from experts, common questions we’re asked about nutrition, and more.