In this video, Dr. Joohi Jimenez-Shahed, movement disorder specialist and Medtronic deep brain stimulation (DBS) programmer speaks with us about what it means to program a DBS system, what to expect at your first and subsequent programming appointments, how long it takes to find the right amount of stimulation for her patients, and more. Visit www.medtronic.com/dbs to learn why Medtronic DBS makes sense. To be notified of more videos like this, don’t forget to subscribe to our YouTube channel.
Topics discussed include:
- Person living with Parkinson’s first diagnosis and progression
- Caregiver experience
- What was the process of choosing DBS?
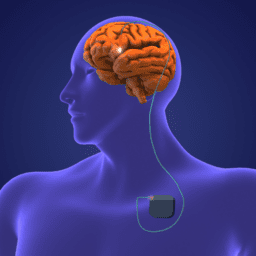
- How does DBS work?
- What happens at initial programming appointment for Medtronic DBS?
- How long does initial programming take?
- What side effects do you look for when programming?
- What should people know about DBS from a patient perspective?
- How do programming needs change over time?
and more. If you’re curious about how DBS programming works, watch, listen, or read below.
The views and opinions expressed in this program are those of the speakers and do not necessarily represent the views or positions of Medtronic.
You can download an audio file of this webinar here: Audio Medtronic DBS Programmer .
You can download a transcript of this webinar here: Transcript Medtronic Programmer and Patient .
Note: This is not a flawless, word-for-word transcript, but it’s close
*While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.