We are excited to announce the research we’ll be funding beginning in 2021:
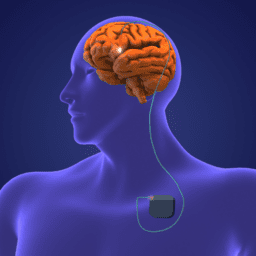
Removing Barriers to Deep Brain Stimulation Surgery
for Women with Parkinson’s Disease
Led by Dr. Michelle Fullard from the University of Colorado, the research team seeks to 1) elucidate the barriers to deep brain stimulation surgery for women and 2) develop evidence-based decision aids and a DBS Ambassador program to address these barriers. The central hypothesis is that women’s informational needs are less often met and that a gender-sensitive intervention will improve decision readiness and satisfaction with the decision-making process.
We are thrilled to be part of moving this important work forward.
Want to know more about Deep Brain Stimulation, these resources are for you.
We also want to update you on a research grant that recently came to a close:
Community-Based Cycling Classes
for Slowing Parkinson’s Disease Progression
This research, led by Dr. Jay Alberts and Dr. Anson Rosenfeldt, sought to discover if Pedaling For Parkinson’s (PFP) (an existing, low-cost program hosted by YMCAs) could slow Parkinson’s progression. The project also aimed to identify which individuals respond the most (more slowing of Parkinson’s progression) to this type of exercise. This project built off Dr. Albert’s earlier work funded by the Davis Phinney Foundation and represented a translation of clinical research to everyday life. Although the pandemic hit this team hard, they were able to transition to virtual visits and virtual PFP classes in order to keep the research moving ahead.
 Results
Results
Disease progression was examined using the MDS-UPDRS III score, a score of global Parkinson’s motor function. Due to the limitations of administering portions of the MDS-UPDRS III remotely (i.e. the rigidity and postural stability components cannot be assessed), 6-month MDS-UPDRS III scores were examined. To truly capture disease severity, the MDS-UPDRS III score was performed OFF of Parkinson’s medication, operationally defined as withholding PD-medication for 12 hours prior to testing. Average baseline MDS-UPDRS III scores were 36.02 (12.09) points. Following the 6-month observational period, average MDS-UPDRS scores fell to 32.23 (11.35).
Why this matters
Parkinson’s literature reports annual increases in (MDS)-UPDRS III from 3.2 to 8.9 points. These data indicate that individuals who regularly participate in a group cycling class may experience a slower rate of disease progression than those who do not. The results provide a foundation to move forward with larger clinical trials that directly examine the impact of moderate to high-intensity aerobic exercise. (Here’s one study looking at this right now.)
What this information means for you
During the final months of the study, the landscape of the world changed drastically. With the closure of gyms around the country, the cycling data collected have proven extraordinarily important in promoting exercise and physical activity in the home environment. Participants in this study demonstrated that individuals with Parkinson’s can be self-motivated to exercise independently at moderate to high intensities on a regular basis without individual oversight from a health care professional.
Thinking about riding a bike? Here are a few resources for you:
What Cycling Options Do I Have when Space and Balance Are an Issue?
What You Need to Know About Cycling and Parkinson’s
Cycling and Parkinson’s: What We Know (and are learning) So Far
Paused Research
Due to COVID, some of the research we funded has been paused. Updates and results will be forthcoming once it’s safe for everyone to reconvene their work.
Innovative Nutritional Therapeutics – In this 12-month project, Dr. Mark Haub of Kansas State University and his team are examining the impact of probiotic supplementation, paired with vitamin B3 (a precursor for dopamine production in the brain), on motor and non-motor function, constipation, quality of life, gut microbiome, and blood levels of Levodopa (indicative of medication absorption) among people living with Parkinson’s.
Colorado Oral Strengthening Device – Elizabeth Cuadrado and her team are partnering with bioengineers to refine and test an alternative to an existing high-cost product to boost tongue strength, which is integral in our ability to swallow. The team at UCD has already prototyped the Colorado Oral Strengthening Device, which is made from silicone and used by compressing it between the tongue and roof of the mouth. This device could be made with multiple levels of resistance akin to exercise bands.
This team seeks to refine the device to elicit the same improvements seen with the current high-cost device. The Colorado Oral Strengthening Device has the potential to help people living with Parkinson’s sustain their ability to swallow for eating and drinking.
SMART Cycling Computerized Controller – Dr. Angela Ridgel of Kent State University will develop and test SMART (Speed Manipulated Adaptive Rehabilitation Therapy) cycling. Her team will develop a computerized model for use in a SMART controller that can be mounted on the chassis of a stationary motorized bike. This controller will use biomechanical data from the rider to automatically adjust bike operation to alter cadence, power, and heart rate during a cycling session and across sessions. Dr. Ridgel and colleagues will also measure the impact of the SMART controller by monitoring motor function and quality of life of people living with Parkinson’s over 12 exercise sessions in 40 participants.
Want to Help Us Fund More Quality of Life Parkinson’s Research in the Future?
We would love to be able to fund more studies so that we can move research forward that will have an impact on people living with Parkinson’s TODAY. We can do so with your help. Please make a donation to our research fund here.