[NOTE: Do you enjoy our YOPD Council sessions? Let us know what’s top of mind for you or any questions you’d like to ask panel members by filling out this form.]
One of the most common questions we’re asked is this: “What should I eat now that I’ve been diagnosed with Parkinson’s?” The answer is that there is no one answer. Just as each person with Parkinson’s experiences different symptoms, each person reacts differently to different types of diets. During this session, our panel members, along with Marty Acevedo, a registered dietician who is living with Parkinson’s, will talk about how food is medicine.
You can watch the video below.
To download the audio, click here.
To download the transcript, click here.
(Note: This isn’t a perfect transcript, but it’s close.)
Melani Dizon (Director of Education and Research, Davis Phinney Foundation):
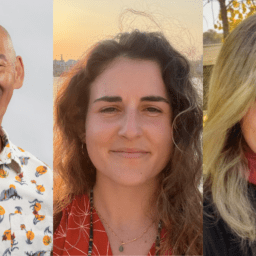
Today we’re going to be talking about YOPD and nutrition and we have our regular council members here. We have Kat Hill who is from Oregon from a beach camping right now which looks absolutely lovely. Tom is here, Kevin is here, and Heather is here. Hello everybody, and our special guest today is Marty Acevedo, and she is a registered dietitian. She has so much information on nutrition, and we are really excited to have you here today Marty, thank you so much for being our resident, all things nutrition.
Marty Acevedo, MS, RDN (Davis Phinney Foundation Ambassador, Registered Dietician): Thank you.
Melani Dizon:
Great. So, to get us started. Nutrition is a huge topic, and it is something that is, nutritional choices that people make are so personal. They maybe are based on health reasons maybe they’re based on moral reasons maybe they’re based on just taste reasons whatever it is but it’s a very personal experience and so we’re not here to tell you, you should eat this way, or you should not eat that way, or this is the only way to be healthy. Today we’re just going to talk about the sort of biology the physical aspects of nutrition what it’s doing to your body what it might be doing with your medication, your energy. Then the council members are going to talk about their personal experiences what’s worked for them what’s not worked for them. And we hope that you guys chime in with your experiences as well and any questions that you have, we have an expert here and we can’t wait to get that expertise from her on all of your questions so feel free to throw them in the chat. Marty, the first thing I want to know, first of all Marty is an ambassador as well, and she spent a very long time she has like a 30-year career in nutrition so I would love to hear from you Marty, on what got you interested in nutrition and what role did it play in your career?
Marty Acevedo:
Well, I was always interested in science and math that’s kind of how my brain works and loved food so I kind of put the two together wanted to work in a hospital but didn’t want to be a nurse, so chose nutrition and became a registered dietitian after college and spent the next 30 plus years of my life managing the nutritional needs of critical care patients in the hospital. Also was involved with leadership and trying to get myself to understand that what they did everything they did with preparing food for patients, it really impacted the patient’s ability to recover from illness and injury. So that’s who I was, that’s basically what I did.
Melani Dizon:
Yeah, so you were a medicine doctor, a nutrition doctor, right? Medicine is food. So, you had all of that background and so much expertise when you were diagnosed with Parkinson’s, did you change up your diet, what did you do?
Marty Acevedo:
I did not guys always felt that I needed to live my life by example, because if I was not following, you know eating the right things and making good choices, using moderation and my decisions that I wasn’t going to be a very good example for people I was talking to.
What I did do was live a more healthy lifestyle and incorporated daily exercise into my lifestyle and I think that’s really important to note that you don’t, people don’t, I didn’t really go on a diet because people go off of diets I changed my lifestyle to be more healthy for lifelong.
Melani Dizon:
Great. I would love to hear some of you all share your experiences around how food has impacted either your motor symptoms non motor symptoms, anything like that. Does anybody have any experience with trying to experiment with different things? Heather.
Heather Kennedy (Davis Phinney Foundation Ambassador, YOPD Council Leader, YOPD Women’s Council Leader):
As someone who also has celiac disease like the late Tom, our hero Tom, the gut microbiome is crucial to us, not only processing our medications, but also our overall health. So, since nothing happens in a vacuum, we’re talking about overall healthier this, this can be a useful conversation to everyone. By finding more nutrient dense foods that are specifically good for our own systems and keeping diversity, which is important in everything in our food, we will be doing okay and Marty is going to talk more about that I’m sure so I’ll leave it to the experts to give us the details.
Melani Dizon: Kat.
Kat Hill (Davis Phinney Foundation Ambassador, YOPD Council Leader, and YOPD Women’s Council Leader):
So, when I was first diagnosed, I was trying to avoid starting medicines right away so I tried to look at the things I could impact myself in how I was feeling and taking care of myself, and like Marty I had a pretty healthy diet but I did do some food journaling and journaling of symptoms, to see if I could impact the way that I was feeling based on what I was putting in my mouth.
And while I noticed what I was eating didn’t seem to have a direct effect, like on my tremor. I did find that it helped a lot of my fog brain symptoms, and also headaches and hurt burn. So, even though some of those may not be directly related to Parkinson’s, it’s directly related to how I was feeling. And so by eliminating or really decreasing the amount of gluten, for me, and again I’m not promoting any diet, I’m not promoting anybody change what they’re doing, but for me personally, it really decreased the amount of headaches that I would get and I had a lot of migraine headaches for many years, and it also completely got rid of my acid reflux. So that was really good learning and I’ve kind of tested it a few times. I’ll go kind of on a “oh I’m going to try just eating, what everybody else is eating for a while,” and sure enough, both the headaches and the reflux come back. So, I’ve done less and less experimenting and just kind of stick with a mostly gluten free diet. Unlike Heather I do not have celiac, so I do not get ill immediately, but I do over time find an accumulation of that. And I try and general to eat the foods that I can pronounce. Or foods that I understand what’s on the label. It’s just been a really good way for me to eat.
So it was trial and error and my own experiment, but I love that we’re having this conversation. Thanks for being here today Marty with us.
Melani Dizon:
Yeah, absolutely. Tom.
Tom Palizzi (Davis Phinney Foundation Ambassador, YOPD Council Leader):
That’s good points that Kat makes there and course Marty as well, and Heather. I think we’re all kind of into this how it affects us individually, of course, this is the nature Parkinson’s but when I was first diagnosed, I instantly started reading about Parkinson’s disease and it had all this stuff about not eating protein so my doctor about that and she said no, that’s not going to really come into play until you start taking meds.
And she said, don’t get too wrapped up in the eating thing until you get a little further along in other words, she said just keep your diet the same if you’re eating healthy already. And we do already eat fairly healthy.
And she said, then it’s things you’ll notice things that will change it and sure enough, I really have a lot of effects from things different things that I eat, so, we eat far less red meat today than we ever did before, or than we did before, and different things like that so I do react today, because I take a lot more Sinemet than I did years ago to the effect of protein so that’s become, I’ve become cognizant of those things but again I think the point I’m trying to make was what my doctors stressed and he was, take a day by day, as you go along because things are going to change, you’re going to change all the time.
And you may change your diet quite a bit. The other thing that I did that was really, had a pronounced effect, was starting to take probiotics. And I think, Heather brought it up earlier the gut biome part, that totally changed things. I mean it really changed the landscape quite a bit. Now the only thing that I can’t seem to live without that still impacts me, is peanut m&ms, so I got to put up with a little bit of discomfort just because I like peanut m&ms.
Marty Acevedo: No bad foods.
Melani Dizon:
Absolutely. Yeah Marty, no bad foods. Kevin, what about you?
Kevin Kwok (Davis Phinney Foundation Board of Directors member and YOPD Council Leader): Yeah. So I have the luxury of having a girlfriend who’s very involved in not only what you eat but the sourcing of how you get it. So she’s very big on to grains and understanding the source of certain grains and what are more natural. And more recently I’ve gotten very involved in you know the role of pesticides and how it affects the food system, and the actual how we could possibly even, not prevent Parkinson’s but there’s an implication that certain foods exposed to certain chemicals can actually increase the risk of getting Parkinson’s. And so I think that there’s you know, Tom, I know you said that you started thinking about it more after, but we may actually be doing some good to our society and our pre-brethren before they get Parkinson’s, if they look at it more holistically.
Melani Dizon:
Agreed. Yeah, so I want to share a comment that Carl, hey Carl Rob, how are you, and he says I felt better with my YOPD when I went vegetarian, my meds works better in my digestion improved being protein sensitive I do try to eat my most dense protein foods like tofu eggs and beans until the evening meal.
Yeah, Thank you for that. Thank you for that Carl. Let’s see. Did anybody else have anything on that on the motor thing I want to talk a little bit about non motor and how you feel, how your food impacts your non motor symptoms. Can anybody speak to anything that’s like oh gosh when I do that, I’m…
Tom Palizzi:
I think mostly I’ve notice it affect the mental part or the non-motor, I’ve had very little impact because I don’t have much of a tremor, so I had very little motor impact on my diet, other than you know slowness of gait and things like that because I’m experiencing a deeper OFF time because I ate too much steak or whatever, which I don’t do anymore so yeah but these days if I eat too many m&ms I get cloudy, so.
Heather Kennedy:
Well, a man without a vice is a dangerous man so you have to have something.
Tom Palizzi: Precisely.
Heather Kennedy:
Who are these maniacs who do everything perfectly healthy, they scare me a little bit.
Melani Dizon: Kevin.
Kevin Kwok:
Yeah, I’m curious to hear Marty’s you on this but it’s not exactly a food group it but it is more of a vise to the peanut m&ms that Tom was talking about is the role of alcohol.
Because if I have now one drink, just even a half a beer or a glass of wine, there are times I almost feel completely inebriated, and I realize I’ve only just had a sip, right.
But my, my whole function slows down, my walk, my gait is completely off, my balance. I mean, you would have thought I was, you know, a wino on the streets right and literally if I got pulled over, I’m sure a policeman would say, you know you gotta go right to jail, there’s no way you should be there. So Marty what is this inebriated state, is this just we’re destined to it now as we progress?
Marty Acevedo:
I’ve always said that if I was ever pulled over regardless of my level of alcohol in my blood that I would be arrested for drunk driving or driving under the influence because I get a tremor when I’m anxious and can’t walk in a straight line, you know that type of thing. So I think it must have something to do with the dopamine production in our brain and then once we have been diagnosed, and we take in alcohol, we’re all different, people tolerate alcohol at different levels, based on our own chemistries but as we progress perhaps, we are less able to tolerate the alcohol that we do take in.
I’m not exactly sure of the the physiology and the brain chemistry there, but some people tolerate alcohol just fine and others don’t. So you kind of have to journal as Kat said and see how it affects you and go from there. As far as alcohol is concerned, there are some good qualities of some types of alcohol like red wine has resveratrol in it that can help with antioxidants and reducing inflammation and may be neuroprotective.
I’m not saying to go out and start drinking I mean that’s not something you should do, but to use moderation in all things and being cognizant of how it affects you is really important.
Melani Dizon:
And I think, you somebody else had asked about coffee, I think it’s very similar. I mean, we all have a different way of metabolizing coffee and alcohol, some people metabolize it, no problem whatsoever.
My husband is Asian, and he has the very common sort of alcohol allergy, and he has one, I can tell how many drinks he’s had, I’m just like, he’s not drunk or anything, but he has that allergy he does not metabolize alcohol well.
And so he gets very red and blotchy immediately and, but at the same time he can drink coffee at nine o’clock at night and sleep like a baby and if I had coffee, even if I had just caffeine, I’d be up for seven days. So, you know, everything is different so if you’re you know asking about coffee or asking about alcohol please, you know, do the experiment figure it out, see, see what happens to your body and maybe even do like a chart where you’re saying, where’s my energy, how is my sleep can I exercise like what am I like the day before do I feel strong do I feel clear in my mind, and, you know, do a little week long experiment, Heather did you want to chime in here?
Heather Kennedy:
Yes, I just wanted to echo the sentiments of what you’re saying, but also what Pam Burnett, I believe one of our listeners was saying about our it exacerbates, alcohol specifically, exacerbates the effects of the drugs so it’s like every for every one you’re basically drinking too so double it up when you do your math, even if you’re just going by blood alcohol level, it doesn’t matter.
And I wanted to add, I happen to know some people in law enforcement so in that the last time there was an open-air fair in our area way before covid by the way we had what’s called the Lafayette Arts and Wine Festival and I asked him to test me as I went in and I was really OFF and shaky. And then I asked him to test me again, and these are sobriety tests by the way, after I had two glasses of wine and walked around the sun, guess which test I failed?
Melani Dizon: The first one.
Heather Kennedy:
You bet. Completely failed. Couldn’t walk the line right couldn’t do that, you know, count by sevens couldn’t say the words backwards, was slurring, shaky.
And I had some people watching who were kind of amazed by this because for a population that is often confused with addiction. And you know how differently addicts, or people who have addictions are treated from people who have neurological disorders, both diseases. We don’t want any more of that so to have that one glass just remember it’s two.
Tom Palizzi:
Alcohol had a big impact on me early on, probably because I started more with the citalopram, the anxiety medication so that drove me off alcohol completely for about five years.
And then just in the last couple of years, I started having a beer again once a while I still want to have a beer maybe once every other week or so just because you know we’ll be out with friends or whatever, but I notice it doesn’t impact me hardly at all anymore, I mean I’m sure it has an impact but not it used to. I used to get really cloudy and really fuzzy, and it was not a good thing, so I just quit all together for a long time.
Melani Dizon:
Kat, were you going to say something?
Kat Hill:
I just want to say Marty, you’re probably going to touch on this but but hydration, I think is really really huge in what we’re talking about. And I think it’s under discussed in that you know how we metabolize our medicine, how we, Heather was saying you know being out and walking around in the sun, alcohol can be dehydrating, certain foods can be dehydrating just, are you going to touch on that Marty?
Melani Dizon:
Yeah, that was my next question.
Kat Hill:
Yeah, so it’s made a big difference in how I metabolize my medicine. I drink an entire eight- ounce glass with every dose of medicine. And it’s funny because camping, I on the way over here I didn’t have a water bottle, and I was like, oh, there’s I need to double up when I get here so anyway, I’m glad you’re going to talk about it Marty.
Melani Dizon:
Yeah, so Marty let’s talk about those sort of in context with meal timing and hydration and some of the questions around protein and that kind of thing.
Marty Acevedo:
Okay so protein competes with carbidopa/levodopa for absorption in the gut. And it also competes with amino acids for transport across the blood brain barrier into the brain where it does its work. So some people have a sensitivity to that and often you don’t have it when you first start taking carbidopa/levodopa, but you develop more of a problem with it later on as your disease progresses.
So most people recommend that you not take your Sinemet or Rytary or whatever, with protein containing meal or you take your medication 30 minutes before a meal or snack containing protein or an hour or two after.
But it’s important not to limit the protein in your diet because you need the protein and calories to sustain, to have energy, to fight fatigue, to keep from losing weight and losing muscle mass. About hydration, Kat’s right, an eight-ounce glass of water with every time you take your meds is really important, you need about 64 ounces of water a day. And that’s two liters, that’s a good way to judge it, it’s to about two liters of water and certain types of liquids are dehydrating, caffeine, alcohol, those types of things are, so you wouldn’t want to really want to include that as part of your fluid intake. Water’s the best, but you can use carbonated things, carbonated waters, that type of thing, flavored water. I don’t really like to taste some water but if it’s ice cold and it has a slice of lemon, I’ll drink it all day.
So that’s what works for me.
Melani Dizon:
Great, I also wanted to mention. So Steve, our usual panelist, those of you who are usually here are probably missing him as we are, but he had something to share and I just thought it was worth sharing so he said as our Parkinson’s progresses our sensitivity to timing our meds with meals and protein changes, for him now it has gotten to the point that if he is doing anything that he really needs to be ON for after a meal that contains a high amount of protein like chicken, eggs, et cetera, he buffers at least 90 minutes before after medicine to allow his medicine to really kick in, if he’s eating a meal that’s maybe more carb based he gives it 45 minutes and that seems to work well.
Let’s see. He did say it didn’t bother him in the earlier stages of his Parkinson’s but in the past five years, he has to be much more disciplined than he used to be, and because the situation is so important, and the importance of protein in our diets in a really smart well-planned diet is super important. So I think you know he’s just mentioning it might not be what it was when you first started out, but if you start to notice and maybe your medications aren’t working maybe you’re OFF more than you used to be OFF maybe timing is a good place to start with, looking into that.
Marty Acevedo:
Another thing that can contribute to your meds not working as well as nutrition related is constipation, because if you’re constipated you often are not able to absorb the medication you’re taking in, not to mention the nutrients that you’re taking in. So hydration is critically important for managing constipation as is exercise and fiber.
Melani Dizon:
Yeah, I would love to talk about constipation. I mean, it’s just so such a great topic, but it is the one of the most popular topics that we get asked about and it’s most frustrating thing in the world. So does anybody on this panel have experience with constipation and what they have done that has worked?
Tom Palizzi:
I’m sure everyone will want to address that right away, right?
Melani Dizon: Yes.
Kevin Kwok:
It’s a moving experience.
Melani Dizon:
This is a safe space; we can all talk about it.
Tom Palizzi:
It wasn’t really a problem until till the last couple years for me and it’s definitely become a recognizable issue for me. And again, water is absolutely key. I’ve always called Parkinson’s dry brain disease. Because one of the commonalities I’ve always noticed whenever I talk to someone with Parkinson’s is I always ask them, did you drink much water before you had Parkinson’s and they say no, I hardly ever did.
And I really think that plays a huge role in how the disease manifests itself in all of us. But again, I think, you know, that water is going to be the source of a lot of your solution to solving issues and dealing with issues.
A good friend of mine, a pharmacist, I was talking about this once, and he was like, dude, don’t you understand that most medicines are designed to dissolve in water, so why wouldn’t you take water bunch of water with your pills?
Melani Dizon:
Does anybody have the memory of their parents when they were young, telling them, don’t drink water after like you take your meds, like, I just remember as a young kid they would be like, especially cough medicine or something like that, they’d be like don’t take the water and I got so trained not to take the water after, which is absurd, like now I’m just like chugging it, but I think it’s funny, right, what we, the wives tales.
Kat Hill:
Well I think if you’re treating cough with an antitussive, or an anticough, there is some coating effect, but that is really the exception in terms of medicines. The rest of them if you picture swallowing a pill with just a little bit of water into your stomach. It’s not like that stomach’s filled with all kinds of fluid to help dissolve and break down the pill.
So picture putting it into a dry tummy, or stomach, and you’re not going to digest or absorb it well without that water and so maybe replace what you’re thinking about water maybe with that and pills, you know, they’ve done studies where somebody’s taken a medicine and they’ve done an endoscopy where they go down with a camera into somebody’s stomach and intestines and sometimes they’ll see a little tablet just stuck to the wall of the stomach and sometimes for visual learners it helps que us, like I’m always thinking about that. Oh, my Sinemet’s going to be stuck right here I just know it I better get some water and flush that down.
Melani Dizon:
Yeah, absolutely. Heather.
Heather Kennedy:
I just wanted to add that with gastric emptying, and the gut motility, that is the answer to having the meds cross the blood brain barrier. So sometimes, as you said, oftentimes, protein will block the absorption.
I find if I eat anything with my first few doses, all I can really have is coffee maybe a few bites of toast or it won’t go anywhere for a while in the morning, especially, so you have to sort of feel how that is for your body and your timeline.
What I would also mention is the gastroparesis I think it’s called that is sort of caused by the slowing that the slowing of our digestion sort of happens over the course of the Parkinson’s journey. It’s really fun, it’s just one of those really fun things you know, that not only drains us of our energies and slows us way down, like Tom was saying if you eat a meal with a lot of meat or something it’s slower to digest, but it will keep us from enjoying everything it’s not just the Parkinson’s symptoms it’ll get worse it’ll be everything they’ve done studies where after people have been put in to psychiatric care for a lifetime, people who are labeled mentally ill and have different illnesses. They’ve done a study on them. And when they do their biopsies and when they do their post ops and everything, they all share one thing in common, gut problems. Every single patient, so it does cause non motor symptoms as well, and foggy thinking, and even mental illness, so take care of your gut.
Kat Hill:
So I wanted to answer the question, sorry. The constipation part. So I’m willing to throw it out there when I travel, or I’m not eating my regular diet is when I can have troubles with constipation and so what I notice when I’m traveling is I’m not eating as many raw foods, apples, oranges, things that don’t travel as well, things that get mushy in my pack. So I try to be really really good about water, exercise, and roughage in my diet and if I pay attention to all of those things, I seem to be able to avoid troubles with constipation at least at this stage of the game. Knock on wood. But it’s like raw, whole, foods, peelings…
Tom Palizzi:
That’s really good point Kat, and I think I’ve experienced exactly the same thing that you’re talking about and you too Heather. And the other thing about water with your with your medications, is you got to get it to your gut first and that takes, in the morning you’re dry, so if I don’t take my pills with a good glass of water, or two, I can feel I’m not getting down there and then like you Heather if I eat something beforehand, a bagel will to stop the process so I always eat after I taken at least 15 minutes to half an hour after I take my meds. First thing, I go to the bathroom, the meds go down, two glasses of water. Just make sure they get there. If I start my day that way, it’s a good day.
Melani Dizon: Kevin.
Kevin Kwok:
I’m curious, I want to ask Marty this question, are there such things as pro-dopaminergic foods? You know I’ve heard like for instance eating raw egg plant actually can result in the formation of more dopamine but is that more of just a myth or is that real?
Marty Acevedo:
I’m not aware of anything that’s pro-dopaminergic, like what you described, eggplant is a nightshade type of vegetable and those do have some antioxidant/phytochemical type properties so maybe that’s what’s helping with that because those are the things in the Mediterranean diet that we know are helpful with inflammation and can be neuroprotective so maybe that’s what the process is there.
I just wanted to mention also that not everyone with Parkinson’s has to deal with constipation, there is a subset that actually has something called irritable bowel syndrome/diarrhea or diarrhea and constipation and they go back and forth.
So some of us, myself included, I don’t have an issue with constipation unless I take a certain medication. So, you know, we have to deal with diarrhea and other things that are intolerant to certain things like gluten in some cases or dairy, lactose in other cases.
And then just you know regular eating can cause problems so that’s why hydration is important with that as well as is fiber as is a good balanced nutritious diet that’s based on moderation and balance.
Melani Dizon:
Right. And we can’t talk about constipation without talking about exercise so one of the best ways to get things moving, is to start moving yourself. I want to just share this comment from Angela Rob, she says, autonomic dysfunction seems to play a role in reducing the thirst mechanism for some people. So as a care partner I do help Carl by queuing for water consumption I think that could impact folks at any time during the YOPD continuum. Yes, absolutely. And I love that idea of just queuing for water and whether that’s something that you, you know, you have on your own, you have on your phone. You’re just always taking a bottle with you, or you have a care partner who’s gonna say hey guess what, it’s time to drink, that’s something to keep in mind.
I wanted to talk a little bit because you mentioned the Mediterranean diet and we often have lots of questions and lots of people experimenting with different diets, and they say is the keto diet is best or vegan diet or vegetarian or whatever so what is your, what is your thought on those diets and since you’re not a diet person, the Mediterranean diet I always give a disclaimer and say that’s actually what it’s called, but we don’t like to say the diet we like to say nutritional choices.
Because we want it to just be something that’s, you know, you’re always on but Marty, what about all the different diets out there?
Marty Acevedo:
Well, Mediterranean lifestyle is what I like to promote, which includes exercise, plenty of water, I’m getting out my sun a bit and the diet it’s based on antioxidants and phytochemicals fiber and that type of thing. There are other things that people try, Kat has benefited from gluten free diet as has Heather because of celiac disease. People are intolerant or have sensitivities to certain types of properties in the foods we eat, so it’s good to identify those by journaling and that type of thing. There was a push for people with Parkinson’s to maybe consider a keto diet, a ketogenic diet and there was a study done by people in Samoa, where they followed a strict ketogenic diet was about 92% fat and a little bit of protein and almost no carbohydrate.
They did very well, their Parkinson’s symptoms improved for the 28 days they were on the diet and again for another 28 days, after they went off the diet.
But that was five people, in a very isolated area and it’s very challenging to follow that diet, you have to follow it 100%, you can’t vary from it at all it’s a diet that’s used for kids with seizure disorders and it’s tends to work for them as well so that’s what the basis for that is. Vegan, vegetarian diets are great, as long as you make sure that you’re getting adequate and appropriate types of protein.
They’re kind of based and on a Mediterranean style of diet. There are lots of vegan and vegetarian foods that are not healthy. My daughter’s vegan and she knows every single fast food, junk food, type thing that’s vegan, like Oreos and Doritos are vegan so you have to be careful with that just because it’s healthy doesn’t mean that everything about it is healthy.
Melani Dizon:
Yeah. And can we talk about how a Dorito is vegan? It’s nacho cheese, what is going on? How is that possible? Let’s just all consider how terrible that is. And a white filling. I don’t know it just seems to be dairy in there.
So, this is an interesting tip. Jackie, she’s a music therapist, she works for the Davis Phinney Foundation, and she said a tip I used for patients needing water in post-operative recovery was to listen to a song and take a drink of water every time they heard a certain word. So if you’re somebody who struggles, give yourself that challenge and give yourself a little a trigger, each time you want to, you need to drink some water. Someone says, can you speak to dairy in their diets? And what about intermittent fasting? So dairy, I want to have Marty talk about that, but again like all of these things are so personal.
Some people have a really really hard time metabolizing dairy some people have no problem whatsoever so let’s talk about that, Marty.
Marty Acevedo:
So, there have been studies done on dairy and the as being a cause of Parkinson’s is the relationship there that has been established through some observational type studies where people actually did surveys so that they drink milk or dairy and that type of thing but there’s no real, the research hasn’t shown any direct implication with Parkinson’s caused by dairy, or that taking dairy and will cause your Parkinson’s to worsen.
That said, there are many of us, myself included, who are lactose intolerant and have significant GI symptoms, when we take in dairy, or anything, cheese, milk, ice cream, those types of things. So you have to be careful for that, so it’s very individualized you know just like Parkinson’s is different for all of us, so is the way we metabolize foods and the nutrients that we take in.
The other thing about milk is I noticed someone in the comments is that it made their phlegm thicker, the fat in milk can cause that to thicken up so if you if you just, if you’re able to tolerate milk to use a low fat or nonfat type of milk to open up the secretions a little bit.
Melani Dizon:
Great, any… Oh yeah, Kat.
Kat Hill:
So, because I did a lot of reading about the inflammatory aspects of dairy, I have found it fairly easy to shift some of my diet to nondairy substitutes and I’ve been really happy with those. There’s almond and cashew-based yogurt, that I really like. I tend to, what else, there’s a couple things that are harder to substitute but I don’t really find that I miss it very much. I still have an occasional ice cream, real ice cream, but there are some great nondairy ice creams also again cashew is my favorite because it’s really creamy. I find that because I don’t taste as well because of the Parkinson’s and losing the smell that texture has become more important to me, so I’ve done a little trial and error and have found some substitutes that work really well for me.
And I find the same kind of thing with less gluten, I’m not as foggy brained. I’m not as phlegmy, and you know for what it’s worth, I think there’s some great nondairy substitutes out there.
Kevin Kwok:
Can we talk a little bit about this issue of not being was smell, how it affects taste, because I have friends who tell me let’s not waste a good wine on Kevin, just give him the cheap stuff, because he can’t taste it. And I swear I can taste good and bad wine. I can taste the quality of foods too. So what’s this issue of hyposmia affecting smell and taste?
Marty Acevedo:
Well when you can’t smell something it does affect the way you taste things and also taste is impacted by Parkinson’s, it impacts our ability to taste sweet and salty, that type of thing so sometimes people crave sweets when they have Parkinson’s because they just don’t taste it. We take can taste bitter and sour pretty effectively, but the other things are impacted. I still have an intact sense of smell so I can’t really speak to that, I’m lucky that way, but taste and smell go hand in hand together.
Tom Palizzi:
That’s interesting because I lost my sense of smell years ago but like Kevin I can still taste things really well, I mean I can taste the difference between like a diet coke and a coke. Yeah, very subtle differences. So, yeah.
Marty Acevedo:
And we’re all different.
Tom Palizzi:
I can hardly smell anything. I smell dirt, smoke, and leather.
Heather Kennedy:
And if you think about the experience of eating it’s a very sensual experience where you smell it first, you salivate like the Pavlovian response, and then you get your gut moving that way right doesn’t that sort of everything moving. So if you’re not smelling it and taking it in, be the equivalent of having, you know, something that is just a color, something to look at but you can’t enjoy its full sensual experience.
Marty Acevedo: Exactly.
Kat Hill:
And I think I find my sense of smell is severely altered, that’s probably a better way of saying it, or my sense of taste is altered, it has changed significantly since my diagnosis and I think it’s impacted by the lack of smell so it takes more flavor sometimes for me to notice a change but I still do have some sense of taste so I like to think my sense of taste is heightened in other ways, perhaps, visually, or kinesthetically, maybe just not orally.
Melani Dizon:
So, all this eating, can we talk a little bit about chewing and swallowing and some of those challenges that people have? What is going on with people with Parkinson’s that are struggling with this and what are some strategies that people can use?
Marty Acevedo:
Well, bradykinesia, slowness of movement, and rigidity both can cause problems with swallowing and the vocal cords as we get older, and as Parkinson’s progresses. Parkinson’s was described to me once as accelerated aging. Symptoms that can happen both with aging and with PD. But so what happens is that if your vocal cords get weaker, and they are muscles and they’re not as able to, they’re not strong enough, they can’t protect your airway when you swallow, at times, so you’re at risk for aspiration or food going into your lungs instead of, or into your esophagus instead of towards your stomach, so that’s a problem for people with Parkinson’s so if you’re having trouble with swallowing and chewing it’s related to yourParkinson’s, your motor symptoms, as well as your autonomic nervous system and being able to, the motility and your gut is reduced, you might want to seek a consult with a speech pathologist, because they can evaluate if you have real problems with your vocal cords or you’re swallowing and identify ways to work around that and strategies so that you won’t have any fallout from that like thicker foods you know mixed foods, like casseroles and sipping with your your chin tucked, no straws, those types of things. It’s really important to address these chewing and swallowing issues because if you’re not able to take in an adequate nutrients you are going to put yourself at risk for losing weight, malnutrition and then that starts a whole cycle of not being able to maintain a healthy lifestyle and having a poor outcome.
Melani Dizon: Heather?
Heather Kennedy:
I’m also noticing that when I’m in public in a really fancy place that’s when I choke. And when you’re choking. Like, there’s a date or somebody there you know you’re trying to impress your date, and you’ve dipped your thick gluten free bread into this like shrimp dish that’s really spicy and you bite it and your throat gets all dry and suddenly you’re like…During covid of course you look like you’re coughing. It’s disastrous. And between that and the incontinence. I mean, forget it.
Melani Dizon:
You’re telling me you’re dating book is not full right now?
Heather Kennedy:
They’re just lining up. At least I had a good laugh, right?
Melani Dizon:
Does anybody else have swallowing or chewing issues and what have you done?
Tom Palizzi:
I saw a physical therapist or occupational therapist for that many years ago. And the best advice she gave me was, you know, to slow down when you eat, which I did naturally because I can’t move quickly like I used to. And, you know, I find myself chewing things up more more completely than I ever did before. And then the best piece of advice you gave me was swallow with purpose. So when you swallow, hammer it down and that’s changed everything and if I don’t, I end up sitting across the table from Heather. Right. I know exactly what you’re going through it. It’s a horrible feeling.
Melani Dizon: Kevin.
Kevin Kwok:
You know one of the things that I’ve noticed over time is I cannot drink out of a bottle. You know it’s that active lifting your head high somehow weakens my muscles for swallowing. And I found that if I actually put something into a glass and use a straw, I’m able to swallow completely.
Marty Acevedo:
Heather made a comment about mindfulness I think that’s really important to practice mindfulness while you’re eating, so that you’re really enjoying the flavor and the taste and the texture of the food and it makes you slow down, so that if you’re, you know it will make you not gobble down a piece of shrimp, I did that you just a couple days ago, a piece of string got lodged and I was doing a Heather. It was just awful.
Kat Hill:
Doing a Heather, I love it. I have trouble. I always find that if I’m having a conversation at dinner which I often am with my family. If I’m thinking about what’s being said, rather than taking the time to swallow that’s when I have trouble, I have to be more mindful about swallowing before responding, or talking so, which is not my strength I will say, but I’m learning. I’m learning.
Melani Dizon:
Does anybody use gum or sugar free suckers or anything to just kind of keep that swallowing going? No?
Tom Palizzi:
I chew gum pretty regularly, and I do okay there. Usually if I choke on something it’s almost exactly the situation that Kat described. I’m having a conversation I’m trying to keep up with everybody, and so you’re trying to swallow it fast and I end up inhaling and it’s ugly for a few minutes and then kind of lasts for a little while to get things sorted out.
Steve just said something about and helping with the drooling and that’s important too. I don’t drool but I can see that working well too.
Melani Dizon:
Yeah, and Betsy says, my person with Parkinson’s always has hard candy nearby. For some people it’s definitely works, careful.
Heather Kennedy:
Although be careful the hard candy. That’s the kind of thing you could swallow if you’re not paying attention too.
Tom Palizzi:
Very true. Very true.
Kat Hill:
And my dad would chime in sugar free is better because he was a retired dentist with Parkinson’s. So, that’s my. There you go.
Melani Dizon:
There’s your PSA. Good job. Okay, from Carl, I think of gratitude when I eat as well, appreciate all the work in the food. Yeah. That’s awesome. Right.
Let’s seem Marty, what did we not address do you think is super important for us to talk about?
Marty Acevedo:
Just the re-emphasizing the importance of hydration and exercise that’s part of our healthy lifestyle, without those two things whatever your nutrition is not going to be, it’s just a piece of the puzzle, and then weight loss and weight gain is very prevalent in our community. People either seem to lose weight or then after DBS like I’m a prime example of someone who gained 20 pounds, just like that, and my diet, what I was eating didn’t change I was exercising more but still gaining the weight, because I think my resting expenditure of my energy went down because I didn’t have that internal tremor any longer and I wasn’t dyskinetic any longer, so that all shifted. So that’s something to think about.
I would do DBS over in a heartbeat, no matter what my weight was going to be but you have to be mindful, again, that word, what you’re eating and how your situation is changing because as we grow older, metabolisms slow as well. So, adjust to that, and then the importance of depression and apathy and the ability to eat appropriately, exercise appropriately, drink enough water and all that type of thing. It’s a non-motor symptom that’s not well discussed. It’s something we don’t talk about enough, and I think it really can impact people if they if they don’t feel like doing anything if you’re apathetic, you’re not, you have to really make yourself get off that couch and go outside and do 30 minutes of exercise drink water and eat the right foods.
Melani Dizon:
Right. Heather and then Kat and then Kevin.
Heather Kennedy:
Just quickly, someone had mentioned, what about the drug interactions? There’s one called Reglan, r-e-g-l-a-n, metoclopramide, I don’t know how to say it, that does block dopamine and unfortunately makes Parkinson’s symptoms worse and yet this is regularly prescribed for patients to get their gut moving.
So, always cross check everything with your doctors and remember that your doctors aren’t talking to each other. Right. So you have to be your own advocate, you have to do the work, and cross check this with all the Parkinson’s friends that you have. I just want to add that.
Melani Dizon:
Yeah, and actually can I ask Kevin about that. So Kevin that feels like a real like pharmacist question as well. Is that something that a typical you know person can discuss with their pharmacists to say, hey, you know…
Kevin Kwok:
Yeah, I think most most pharmacists would know you, not so much Parkinson’s issues, but issues like medical clopramide, and its effects on your gut. A pharmacist is always a good friend to have
Tom Palizzi: At least two.
Melani Dizon:
At least two pharmacists?
Tom Palizzi:
Yeah, I have no two friends that are pharmacists and they’ve become best friends because of all that.
Kat Hill:
I just wanted to mention too that, for those of us that are diagnosed around perimenopause, the shift in caloric needs really shift after a menopause and so just being aware of that. And again it’s back to mindfulness, it’s back to all the things we’re thinking about, but you can be eating exactly the same amount of calories before menopause and suddenly need significantly less after menopause. So, that can throw a just an added element of awareness, right, an opportunity for growth of learning, again.
Melani Dizon:
Kevin, what were you going to say?
Kevin Kwok:
Oh, I was just, I have a lot of questions for Marty, but I wanted to know whether or not, that we talked a little bit about foods that might cause inflammation or anti-inflammatory foods, and also are there foods that actually can help with cognition like Lion’s Mane mushrooms or what?
Marty Acevedo:
Well anti inflammatories are berries, fruits and vegetables, grapes, come to mind, whole grains, that type of thing, fish, rather than red meats, turmeric is a really good a has a lot of anti- inflammatory processes, that’s the spice that seasons mustard and lot of Indian food curry, that type of thing. There are other spices Rosemary is a good and good has good properties.
As far as brain foods that I think Heather mentioned sauerkraut and fermented foods kombucha that type of thing, those are all good things that can help to be neuroprotective. Eating a balanced diet, making sure you’re getting adequate proteins, calories and nutrients from real food not from a processed food or chemical not taking a pill but instead of eating real food can all help with making your brain more clear and your cognition intact.
Kevin Kwok:
Do you take supplements?
Marty Acevedo:
I take a multivitamin but that’s it. You know a lot of people will say are interested in taking extra B vitamins and I tell them what you’re going to have awfully expensive urine. Because anything that you don’t use, you’ll just pee out.
So that’s one thing and then the fat-soluble vitamins A, C, and E also have antioxidant properties but if you take too much of them, then you’ll store them in your liver and that can cause other problems as well so if you’re going to take a supplement it should be, you should only take a single nutrient supplement if you’re deficient in it or if you know that you’re having problems.
Kevin Kwok:
What about protein shakes? I do a lot of protein shakes for workouts. Is that bad because it interferes with your medication?
Marty Acevedo:
That’s something that you’d need to journal and see if it’s affecting your symptoms. Are you having more OFF time after you’ve taken a protein shake, it may not affect you at all. There’s no problem with that you know some people say that you need to refuel with exercise, so that’s probably, that could be a good source of refueling
Melani Dizon: Kat.
Kat Hill:
Just wanted to bring up something that we didn’t touch on and that is intermittent fasting. Marty, what are your thoughts about that? Is that something we should be trying, for trial and error, or not?
Marty Acevedo:
That has the same basis and research as the keto diet where you’re actually putting your body and your brain into a ketonic state, which when I was working in the hospital, we really tried to avoid ketosis in our patients because it can be harmful to the kidneys and other organs and it’s not good, the brain needs glucose to operate appropriately. And when you’re in ketosis, it’s relying on fat and glycogen stores, so that’s the premise behind the intermittent fasting.
Some people have found that that’s successful for them their symptoms have improved and, you know, it’s just something that people need to try and it’s on an individual basis, I can’t say one way or the other, there’s not a lot of research that’s been proven on it but if it works for you then go for it. Just make sure that your diet’s moderation, as I always say in all things.
Tom Palizzi:
Yeah, I’ve found just simply slowing down, enjoying what you eat. I eat a lot less because I eat my body recognizes when it’s full at a normal pace. Usually you’re eating and you’re full but you don’t recognize it until several minutes later, you tend to over eat, at least that’s how I used to be, but that’s really changed everything just eating slowly, enjoying what I eat, and that’s really helped me, avoid bloating constipation problems and all kinds of issues so. And I feel really good diet wise, I’ve been doing really well over the last few years, as my body has changed with the different kinds of medications and Parkinson’s has progressed even more so it’s, I’m keeping things in a pretty good balance.
Melani Dizon:
Great. So, a couple of questions regarding supplements and vitamins, should they be taken with medication or separately? Does that have any impact on absorption and then the other question is the best foods to gain weight that are also nutritious?
Marty Acevedo:
With calcium, if you’re taking a calcium supplement you can only take so much of that at a time because it’s not absorbed well if you take too much time, I think it’s like 500 or 750 milligrams of calcium at a time and split that up. As far as it interfering with your other medications, I don’t think so.
But, you know, if you notice that you’re having more severe more symptomatic after taking it then that’s a problem, then note that. Also with gaining weight just having more frequent meals, smaller meals during the day, adding shakes like Kevin does. You know snacks throughout the day, healthy snacks, those types of things, those can always help. You can also use commercially developed supplements like, I won’t promote one over the other, but you can combine them with ice cream or nondairy ice cream to make make things.
One thing we didn’t talk about was the gut biome that Heather had mentioned, we all have bacteria in our gut and most of us with Parkinson’s have certain types of bacteria that are higher in us than other people do so that can contribute to possibly, that’s where we think alpha synuclein starts and goes to the brain and can cause a Lewy Body aggregations so that’s something we need to be aware of and that’s probably a whole other session, just to talk about the gut microbiome
Melani Dizon:
Yeah, and just so everyone knows we are going to actually be talking to Dr. K on constipation and the gut, on one of our main webinars and he’s just so good with that so we’re going to, I think we’re doing that and then in the next month or so, so stay tuned for that. Does anybody have any final thoughts or pieces of advice or anything before we wrap this up today?
Kat Hill:
I just want to thank Marty for coming and I think it’s been really informative I know that I’ve learned a lot. I learned a lot every time I come. Thank you for joining us for sure.
Tom Palizzi:
Yes, Marty, thank you.
Melani Dizon: Thank you Marty!
Show Notes
- Eating nutritiously is an important factor in living well with Parkinson’s, but there is no one-size-fits-all Parkinson’s food plan. Explore different healthy eating plans to find what feels best for you. Panelist Kat Hill recommends keeping a food and symptom journal so you can clearly see what foods are impacting you and how
- As Parkinson’s progresses, bradykinesia and rigidity can cause problems with swallowing, which can increase your risk for aspiration (when material goes past the vocal cords, goes down toward the airway and then filters down into the lungs). Some tip from our panelists to reduce this risk include swallowing with purpose, slowing the pace of your eating, and eating mindfully (which can also enhance the flavor and texture of your food and decrease over-eating)
- Marty says that single-ingredient supplements are only necessary if you know you’re deficient in that vitamin or mineral. Be sure to talk with your physician about any supplements you’re interested in taking before you begin to take them
- There are countless diets and eating plans that are advertised regularly, including the Mediterranean diet, Whole 30, the Keto diet, paleo, and more. Explore what feels good for your body. It may be one of these plans, none of these plans, or some elements from each. You may try utilizing Kat Hill’s method for healthy eating: to buy foods with ingredients on the label that she can pronounce
- Hydration is critical for healthy living and for Parkinson’s in particular. Proper hydration minimizes constipation and helps with medication absorption, among other things
- Protein is an essential part of a healthy diet, but be mindful about when you consume it in regards to your medications since protein interferes with the uptake of carbidopa/levodopa. To help avoid this interference, try to take your medications 30 minutes before or one to two hours after eating a protein-heavy meal
- Life happens, and you may not be able to eat a perfectly balanced diet all the time. When this happens, compensate with what you can control. Kat says that when she’s camping, she tends to eat more processed foods, so to balance that, she drinks extra water and adds extra fiber into her meals
resources and topics discussed
The Science of Parkinson’s OFF
How to Take Levodopa for Parkinson’s
The Science of Parkinson’s Constipation
A Plant-Based Diet for Parkinson’s
17 Most Commonly Asked Questions About Parkinson’s Nutrition
WANT more advice from our yopd council?
You can register for the entire YOPD Council series here, as well as catch up on recent conversations here. We meet on the third Thursday of every month to discuss the unique challenges of living with YOPD. Have an idea that you would like the YOPD Council to discuss? Fill out this form contribute to future topics for the YOPD Council.