Written by Jerry Boster, Davis Phinney Foundation Ambassador
When I think back to the day I was diagnosed with young onset Parkinson’s (YOPD), it remains a blur except for two things – the doctor saying very matter-of-factly, “You have Parkinson’s,” followed by, “I think you would be an ideal candidate for a drug trial that is recruiting.”
With those statements, my future would become an intertwining of these two concepts, one representing the reality of today and the other a hope for the future in the form of a cure. But I’m getting ahead of myself.
I left the doctor’s office in a haze. I had heard and understood his words, but I didn’t comprehend what they really meant. So, while my emotional side struggled to deal with a new reality, my logical side craved information to understand Parkinson’s and the role of clinical trials.

My first stop was the Michael J. Fox Foundation for Parkinson’s Research website. After reading the “Understanding Parkinson’s” section for a while, I decided to take a break and look at clinical drug trials. Appropriately, I found the trials under the “Take Action” tab. After being a US Navy officer for 24 years, taking action and finding solutions was right up my alley. So, I dove in and started reading. I soon discovered a startling and distressing fact: “Across all research, 85 percent of trials face delays and 30 percent never get started because of the chronic shortage of volunteers.”
This made me wonder how many possible cures were left on the chalkboard. Then I got mad. And then I got determined. I told myself I wouldn’t be the one to leave a potential cure behind. I called my neurologist and told him I wanted to join the drug trial, and he called the supervising clinician who quickly reached out to me. And just like that, I was participating in my first drug trial.
I was lucky and started with an “easy” trial. The researchers were testing to see if nicotine was the reason smokers had an apparent later onset and slower progression of Parkinson’s. To test this possibility, I was placed on the nicotine patch (yep, the same one smokers use to kick the smoking habit). I spent two months working up to the trial dosage of 28mg/day, then nine months at the trial dosage, then two months being weaned off the nicotine. Along the way, my Parkinson’s was routinely evaluated by two doctors to see if the nicotine reduced my Parkinson’s symptoms. (It didn’t). After 13 months, I was back where I started, but with an added sense of satisfaction that I was helping to advance Parkinson’s research.
While participating in the nicotine study, I also started taking part in online studies, something I continue to do today. Most of the studies I have participated in are self-observed reporting of my lifestyle, habits, and Parkinson’s condition over time. Typically, my role in these studies is to complete a survey every three or six months. I take the 30-60 minute survey, and I am done until the next time. Most studies are fairly short – one or two years in duration – but recently I received my 23rd quarterly survey link from one study indicating I’ve been participating for nearly six years.
One study that broke this mold was an in-person drumming study that I participated in a few years ago. The goal of the study was to improve strength and dexterity in my hands and arms. Every Sunday for three months, I joined nine other “drummers” in playing an African style drum. While I can say for sure that I will never be another Ringo Starr, the drumming exercises did appear to improve my coordination, strength, and dexterity in both hands and arms.
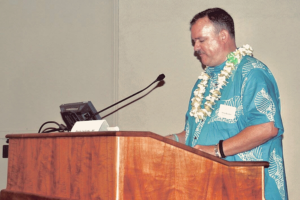 Taking part in these various studies and trials has turned me into a passionate advocate for volunteer participation in clinical trials. Almost every presentation I give as president of the Hawaii Parkinson Association has at least a sentence or two about the significant need for volunteers. “Everybody wants the latest and greatest treatments,” I often tell people, “but the only way to get them is for people to volunteer for clinical trials.”
Taking part in these various studies and trials has turned me into a passionate advocate for volunteer participation in clinical trials. Almost every presentation I give as president of the Hawaii Parkinson Association has at least a sentence or two about the significant need for volunteers. “Everybody wants the latest and greatest treatments,” I often tell people, “but the only way to get them is for people to volunteer for clinical trials.”
In addition, whenever I have a routine appointment with my movement disorder specialist (MDS), I always ask about pending clinical trials and new drug developments. If there are any new and promising clinical trials beginning in Hawaii, we discuss my potential participation. Since the nicotine trial, I had not participated in any trials until 2020, either because I didn’t qualify for the trials or because the medication being studied didn’t fit into my treatment regime (meaning it would probably do more harm than good). However, in the fall of 2020, one of the local testing organizations announced they were recruiting for a Phase I clinical trial for a new neuro-protectant drug. Phase I trials test a potential therapy, procedure, or drug for the first time in a small number of people and typically evaluate the safety of a new therapy. They also often yield information on side effects, effectiveness of delivery method, and appropriate dosage levels.
After receiving clearance from my MDS, I contacted the lead clinical researcher and arranged my intake appointment. It was during that visit that I found out the real cost of participation. Because one of the trial objectives was to ensure the trial drug reached the brain in proper quantities (which is evaluated by measuring cerebral spinal fluid), I would have to donate cerebral spinal fluid (CSF) twice via a spinal tap.
Having heard horror stories from others about the spinal tap process, I was not exactly enthusiastic about participating. In fact, I felt a healthy dose of fear. I discussed my concerns with several trusted friends who provided opinions both for and against the spinal taps (and also provided lots of support). At one point during these conversations, I realized that I had reached an important crossroads. Put quite simply: I had been talking the talk; now, was I going to walk the walk? As a career military officer, I recognized that I couldn’t continue to effectively lead if I wasn’t willing to do myself what I so passionately advocated for others. With that realization, I clamped down on the fear and called the lead trial tech to schedule the first spinal tap.

It turned out that with current techniques and equipment, both spinal taps went very well and were relatively minor events. (I’ve had broken bones that were bigger deals). For the first tap, I was only on the table for about 15 minutes and had no problems, not even a headache. The second tap was more involved; the team put in a flexible catheter that allowed them to draw CSF every hour for seven hours to measure how much of the trial drug was in my system throughout a full six-hour dosage cycle. Again, my body tolerated the procedure fairly well. The only real issue was that they were also drawing blood following each CSF draw, so by the seventh and last blood draw, the veins inside my elbows were getting very sore and tender.
Looking back at both clinical trials, the drumming study, and all the observational online studies, I can say with no doubt that I am glad to have played these roles in Parkinson’s-related research. Today, I remain a firm advocate for volunteer participation in trials and studies, if not for your own benefit, then for that of future people with Parkinson’s. I encourage you to explore the trials available in your area and make the call to volunteer. You never know, you might get lucky and hit the cure “jackpot” during one of the trials. I know, I know — I’m a dreamer and an optimist. But why not give it a shot? I did, and in the future, I will again.
Ready to get involved?
Learn more about research and how to get involved in clinical trials here. Want to support research in a different way? Financial contributions are an integral part of scientific advancement. Consider making a donation to the Davis Phinney Foundation Research Program, and support research that helps people with Parkinson’s live well today.
We are saddened to share that Jerry Boster passed away on Thursday, July 13, 2023
Though you are no longer with us, Jerry, you will never be forgotten. Thank you for being a friend and for the legacy you left to the Parkinson’s community.
If you’d like to learn more about Jerry’s work and help maintain his legacy, visit the Hawai’i Parkinson Association.