
Most people with Parkinson’s begin a course of treatments to help manage symptoms. Treatments often include a unique combination of medications and surgical therapies as well as exercise and other complementary therapies like acupuncture, speech and language therapy, physical therapy and occupational therapy.
In this post, we help you better understand your medication options for Parkinson’s.
Medication Therapy
Medication therapy is an important part of your comprehensive care. Most Parkinson’s medications target motor symptoms and can be extremely effective, especially in the early stages of Parkinson’s.
When medications provide almost total relief from the primary motor symptoms of Parkinson’s, this is sometimes referred to as the “honeymoon phase.” Even after this early honeymoon phase, medications can be extremely effective, especially when optimized by your physician. Optimization of medication means making sure you receive an appropriate dose of your medications to best control motor symptoms.
There are three primary categories of medications to treat motor symptoms:
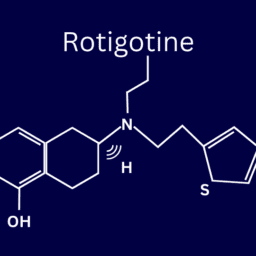
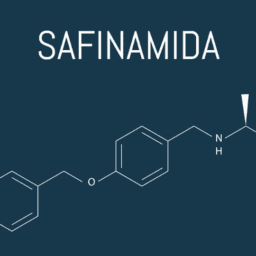
- Dopaminergic medications for movement. Dopaminergic medications replace lost dopamine and can be used to treat tremor, stiffness, slowness and problems walking. These medications may also have a beneficial impact on non-motor symptoms of Parkinson’s related to sleep, mood and cognition. Dopaminergic medications, such as carbidopa-levodopa (Sinemet®), make up the majority of medicines used to treat Parkinson’s and can sometimes be used in combination with each other because of how they impact the body. As Parkinson’s progresses and more of these dopaminergic medications are needed to address symptoms, you may experience motor fluctuations and frustrating side effects of the added or increased medication, like dyskinesia. Dyskinesia is uncontrollable, jerky movements of the arms and legs caused long-term use of levodopa.
- Muscle relaxants and pain medicines for painful spasms and rigidity.
- Anticholinergic medications for rest tremor. Anticholinergic medications are used to block the neurochemical acetylcholine, which can help reduce rest tremor. These medicines do not improve other motor symptoms such as rigidity, slowness or walking problems. Anticholinergic medications should be used cautiously as they can cause side effects such as dry mouth, blurred vision, dry eyes, constipation, memory problems and confusion, especially in people who are older.
Occasionally people with Parkinson’s want to avoid increasing their medications. While there are a number of different reasons for this, there used to be a concern among healthcare providers that certain Parkinson’s medications would become less effective over time. As a result, many adopted a philosophy of “levodopa sparing,” or using the lowest possible dose of levodopa in an attempt to conserve the medication’s effectiveness for as long as possible.
This medical perspective is no longer believed to be true. Numerous research studies have shown Parkinson’s medications should be started as soon as symptoms begin to interfere with your quality of life. Research has also demonstrated finding an optimal combination and dosage of medications has strong potential benefits such as reducing the risk of falls, improving quality of sleep and increasing your ability to exercise.
That said, many people do discover medications are not as effective as they used to be the longer they live with the disease. The reason has less to do with how long you have been using Parkinson’s medications and more to do with the amount of damage Parkinson’s has done to dopamine-producing nerve cells. As Parkinson’s progresses, more nerve cells that produce dopamine die, leaving less and less dopamine in the brain. Most Parkinson’s medications work to replace lost dopamine, but since current medications can only replenish so much lost dopamine, the more dopamine you lose, the less effective medications will be at controlling the various symptoms of Parkinson’s.
You may experience less time when the medications are working effectively (called ON times) and longer, more frequent periods where medications are not working and symptoms return or get worse (called OFF times). During OFF times, problems walking or speaking and other Parkinson’s symptoms like tremor, stiffness, slowness, posture, balance and anxiety may become more pronounced.
As OFF times increase, medications may need to be taken closer together. This can cause dyskinesia, uncontrollable, jerky movements of the arms and legs that comes as a side effect of adding or increasing dopaminergic medication. Sometimes the side effects of Parkinson’s medications can be even more frustrating than the symptoms these medications are trying to treat. If you are experiencing dyskinesia, begin recording when you experience ON times, OFF times and dyskinesia as well as when you take your medications to help you to keep an ongoing conversation with your doctor about the most effective ways for you to use and adjust your Parkinson’s medications.
In most situations, the effects of Parkinson’s medications last a relatively short amount of time and must be taken over the course of the day to maintain the benefits. However, discoveries of new and improved methods of treatment are happening fast and new medications continue to be added to this growing list. Notably, a lot of “new” medications are improved formulations of older medications that enhance their ability to be used by the body and remain in the system for longer periods of time throughout the day, requiring less frequent and sometimes, smaller doses.
Medications for Other Symptoms
There are a number of Parkinson’s symptoms not directly related to movement known as non-motor symptoms. Non-motor symptoms include a wide variety of problems ranging from difficulty with sleeping, depression, apathy and anxiety, changes in cognition and gastrointestinal issues such as constipation and urinary dysfunction. Parkinson’s medications typically don’t directly address these symptoms, but the way medications can improve your ability to move may have secondary benefits that help with non-motor symptoms. For example, if a medication like carbidopa/levodopa allows for more activity and exercise, this often results in better sleep function as well as gastrointestinal health.
However, in situations where there is a troubling non-motor symptom, it is often best to have a conversation with your doctor to see if there are medications that can relieve some of these challenges. For example, your doctor may recommend a medication to address a symptom like depression or neurogenic orthostatic hypotension (nOH) that may provide direct relief to that specific symptom.
In addition, over-the-counter options or other complementary therapies like acupuncture may provide relief for certain symptoms and can often be combined with simple lifestyle modifications to make significant improvements in many non-motor symptoms. For instance, increasing the amount of fluid you drink and the amount of fiber you eat may help alleviate troublesome constipation.
The following non-motor symptoms can be treated with medication:
- Pain
- Hallucinations
- Parkinson’s-related changes in cognition
- Depression, apathy, and anxiety
- Overactive bladder and other urinary issues
- Neurogenic orthostatic hypotension (nOH)
- Many different types of sleep issues including REM sleep behavior disorder
- Sexual health issues
- Gastrointestinal issues such as reflux, constipation and gastroparesis
Your neurologist is likely your first source of information about these types of medications as you consider the best approach for addressing and controlling your symptoms. In addition, physician assistants, nurse practitioners, pharmacists and advanced practice nurses, sometimes called Parkinson’s nurse specialists, can be very helpful as well.
There are new treatments coming onto the market regularly, so continue to discuss with your healthcare providers to assess whether there may be other options for symptoms you are experiencing. In addition, many of these medications can be combined with non-pharmacological treatments to increase your quality of life.













Does part b cover the various speech therapy programs developed specifically for hypophonia due to PD?
Hi Robin,
In early 2018, Congress passed a spending bill that eliminated the Medicare therapy cap, which limited the amount of physical, occupational and speech therapy someone could receive, which was a big deal for the Parkinson’s community. The best way to know how your speech therapy can be covered is to consult with your Medicare representative. They can access your coverage and discuss ways to get what you need. In the meantime, this article may be helpful to you: https://davisphinneyfoundation.org/blog/medicare-coverage-and-parkinsons/
I’m at the very beginning of my life with Parkinson. I live in Italy and I’m 66 years old. My main problems are slow tremor in left hand and slow movement on left feet. Also a little voice during the day. My doctor is waiting to use levodopa because he said that’s not the moment due to small problems. What’s your suggestion? He gave me only 2 cp per day of Mnesis.
Dear Graziano – I would follow your doctor’s instructions. If you do not experience relief, be sure to let him/her know as soon as possible. Your doctor is the best person to handle your medication management.