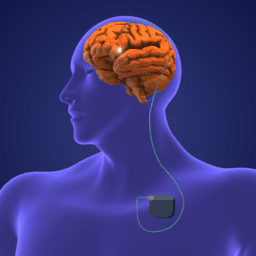
Deep brain stimulation (DBS) surgery is one of the most effective treatments for the motor symptoms of Parkinson’s. And for some, it’s the difference between just existing and thriving with Parkinson’s. During this interview with surgeon Dr. Doris Wang and movement disorder specialist Dr. Jill Ostrem, we talk about the following:
- What DBS is
- The symptoms DBS helps with
- Who makes a good candidate for DBS
- Things to know about DBS batteries
- Asleep vs awake DBS surgery
- DBS “targets” in the brain
- The most important things to know about DBS
- And more
If you’re curious about DBS, watch, listen, or read below.
The views and opinions expressed in this program are those of the speakers and do not necessarily represent the views or positions of Medtronic.
You can download an audio file of this webinar here: Audio Medtronic DBS Surgeon .
You can download a transcript of this interview here: Transcript Medtronic DBS Webinar with Surgeon and MDS .
Note: This is not a flawless, word-for-word transcript, but it’s close
*While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.