Dear Pharmacy Benefit Managers,
As a person living with Parkinson’s, I am writing to urge you to reconsider your recent decisions to move several common Parkinson’s medications to your exclusion lists or step-up medication lists. Doing so has caused heavy and unnecessary burdens on me, many of the people I personally know in the Parkinson’s community, and thousands of other people with Parkinson’s around the country.
I am one of more than 10 million people worldwide living with Parkinson’s today. Each of us experiences it differently, in terms of both symptoms and progression. In fact, in a paper published in The Lancet in April 2021, three of the world’s leading Parkinson’s experts write that because “every person has their own unique Parkinson’s…an extreme notion would be to say that there are over six million different variations of Parkinson’s in the world.”
Each one of the 10 million of us experiences different symptoms, many of which are not visible and even more impactful on our quality of life than outward signs such as tremor and slowness of moment. Each one of the 10 million of us experiences a different rate of progression. Each one of the 10 million of us responds differently to various medications, surgical therapies, and other treatment options.
Nonetheless, for almost all of us, medication is a big part of the strategy. We rely on medication to manage motor symptoms and non-motor symptoms alike. We rely on medication to help us move, work, engage with the world, raise children, give back, stay positive, and maintain our quality of life while living with an incurable, progressive, chronic neurological condition.
What, then, happens to our movement, work, families, communities, emotional and mental health, and overall quality of life when the medications we have come to rely on are no longer available to us due to changes in the formularies you create?
How is our quality of life minimized when a medication like the extended-release carbidopa/levodopa drug Rytary®, proven in clinical studies to greatly reduce people with Parkinson’s OFF times, is classified as a step-up drug that our insurance will only cover after we’ve spent ample time experimenting with other medications not proven to do the same, and that do not manage our symptoms?
What happens to our movement (and all that movement entails) when a medication like GOCOVRI®, the only drug approved by the FDA to treat both OFF times and dyskinesia, is no longer affordable because it has been moved to our insurance’s exclusion list?
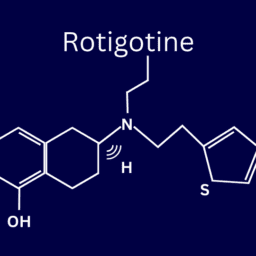
What happens when we walk up to our local pharmacies, where we have gone to pick up our Parkinson’s prescriptions that we have been taking for several years with great success, and are told that our Osmolex ER, or Ongentys, or Xadago, or Zelapar, or Ingrezza, or Apokyn, or Inbrija, or Nourianz are no longer covered?
This is what happens:
- We may have to stop that medication cold turkey, without time to titrate off it. Depending on the medication and what symptoms we are trying to manage, this can be anywhere from mildly bothersome to very dangerous.
- If we do have to stop the medication without adjusting to lower doses first and then experience dangerous side effects, we could end up hospitalized. For people with Parkinson’s, hospital stays require special consideration. Our motor symptoms may worsen, and we might not be able to move as well as we usually can. And because confusion and hallucinations can occur or worsen in the setting of medical stress or as a result of new medications, such as narcotics for pain, or sedatives for sleep, anxiety, or agitation, we may experience dramatic decreases in our physical and mental health and well-being.
- We may have to titrate off the medication that has been working well in order to begin the slow process of using a new medication that may or may not work for us.
- We may have to pay out of pocket for the medication because we have determined, through much tumultuous trial-and-error, that this medication is the only one that will work for a particular symptom that impacts our daily lives. Oh, and this may cost us thousands of dollars. Per month.
- We may have to not only swap out the medication on the exclusion list but also other medications we’re taking to treat our Parkinson’s motor and non-motor symptoms if the new medication we begin has adverse interactions with others in our drug regimens. This compounds many of the other complications we have mentioned.
- We may feel as we did when we received our Parkinson’s diagnoses, unsure of what actions to take to manage our symptoms. This can cause extreme stress and additional anxiety, something that 50% of us already experience while living with Parkinson’s.
- We may experience a resurgence in symptoms that have been under control for some time.
- We may have to have more appointments with our physicians as we work through the process of titrating off one medication (or more) and onto another (or more). Because these kinds of appointments can be time-consuming, exhausting, and stressful for us as people with Parkinson’s, this is more of a burden than it might seem. It is also a burden to our care partners, as well as the healthcare system.
We recognize that there is a process we can follow to request an exception to your exclusion lists. We also recognize how confusing, frustrating, and disheartening this process can be. Even after we have worked with our physicians and their office staff to secure a letter confirming that the medication we are requesting is necessary to our care, the request will almost certainly be denied. If we appeal this decision, our request may be denied once again. All the while, we will likely be experiencing (at best) fluctuations in symptoms that had previously been managed and (at worst) such bothersome symptoms that we end up hospitalized.
A silver lining for the 10 million of us living with Parkinson’s is that Parkinson’s research is progressing. Physicians, scientists, professors, and researchers understand much more clearly now than they did a decade ago how unique Parkinson’s is to everyone, and how personalized treatments are the key to living well with Parkinson’s. Dozens of new drugs are being investigated that might not only treat symptoms but slow the progression of Parkinson’s. We know that our own actions can have a profound impact on our daily lives and our future as we continue this journey.
And yet, we still face countless challenges. We still live with a chronic, incurable, progressive condition that, to manage, takes Olympic-level dedication, willpower, stamina, and support.
You as PBMs could help us—immeasurably—by reconsidering your recent decisions about GOCOVRI, Rytary, Osmolex ER, Ongentys, Xadago, Zelapar, Ingrezza, Apokyn, Inbrija, and Nourianz. You could help us by making the exceptions process more straightforward and easier to navigate. You could help us by listening to Parkinson’s experts and people living with Parkinson’s about how personalized care, and a variety of treatment options, is critical for living well with Parkinson’s, the fastest growing neurological condition in the world.
Sincerely,
People with Parkinson’s