Written by Kris Meldrum, BA ACE, Neuro Wellness Program Lead, Neuro Wellness Parkinson’s Coach
Vetted by Dr. Jay Alberts, PhD, Vice-Chair of Innovation in the Neurological Institute and Neuroscientist, Cleveland Clinic
(Note: This article was originally published in a Neuro Wellness Program newsletter. We received permission from the author to publish here with minor edits to improve readability on our blog.)
The first indoor Genesis Neuro Cycle ride following the three months that the COVID-19 pandemic kept riders out of the cycle studio was actually worse than when we first opened our doors many years earlier. It was so unexpected and jolting. Students (primarily people living with Parkinson’s) with whom I had worked for years were displaying symptoms I had never seen before. It took my breath away. And riding bikes again took all our breaths away. It was like climbing up the biggest hill we had ever encountered. Gone was the optimal 80-85 RPM (the magic revolutions-per-minute that kickstarts the brain to create better motor function) that they had worked so hard to achieve. Watts (strength output) had plummeted. How was this possible in such a short amount of time? And most heart-wrenching was to see them struggling with symptoms they didn’t have prior to COVID-19 showing up on our doorsteps.
This real life scenario reinforces what Jay Alberts’ (PhD, Vice-Chair of Innovation in the Neurological Institute and Neuroscientist in Cleveland Clinic Lerner Research Institute Department of Biomedical Engineering) 2009 landmark research titled “Forced, Not Voluntary, Exercise Improves Motor Function in Parkinson’s Disease Patients” showed in his research findings. Dr. Albert compared two cycle groups of people Parkinson’s: one group riding at a “forced-paced” (exercising at a higher level than they normally would by themselves) versus a group riding at “voluntary-paced” (exercising at their own pace). While both groups improved aerobically, the VE (voluntary effort exercise) group did not exhibit any improvement on the Unified Parkinson’s Disease Rating Scale (UPDRS) motor scores. The FE (forced effort exercise) group improved 35% from baseline. This group also had substantial improvement in their overall motor function—balance, tremor, stiffness, and bradykinesia. Also, the FE Group maintained those benefits up to four weeks after they stopped cycling.

The Genesis Neuro cyclists demonstrated in real time what Dr. Alberts proved in his FE study. When we first started, the majority of the students were riding at cadences between 50-60 RPM and could only ride 10 to 15 minutes on indoor cycle bikes. They were encouraged to ride at their level of comfort but coached to gradually improve over time to ride with forced pedaling. As per Dr. Alberts’ study, the goal of forced pedaling is to ultimately get them cycling at a cadence of 80 RPM and above. While this may sound fast for a person with impeded neurological and physical movement performance, it is actually quite achievable. Remarkably, after six months time, those students who consistently rode each week were able to hit all the sections on their Metric Assessment Rides — including 80-90 RPM, and could easily ride a 45-minute class. One year later, they gained considerable leg strength and power output ranging between 80 to 200 watts.
Then came COVID-19. Everyone’s world was turned upside down. It affected everyone greatly, but none more than people with Parkinson’s and other neurological conditions.
COVID-19 created a great deal of stress on my neuro wellness student. Here is a snapshot of what happens to neuro wellness students when you add major stress to their lives and take away their FE options: They drastically lose their aerobic and strength capacity and capabilities at an alarming rate. It’s what Dr Albert’s research study showed: a four week “window” of benefit would be maintained after stopping FE. This was absolutely true for the Parkinson’s cyclists in my class. They felt good for four weeks after stopping cycling due to COVID-19. However, then they experienced a big drop in those benefits and either a worsening of motor symptoms or non-motor symptoms, or both.
Or, they felt new symptoms all together. Interestingly, the stroke students found the benefits only lasted two weeks before feeling the drop off.
A 2015 study on the “Effects of stationary cycling exercise on the balance and gait abilities of chronic stroke patients” established that stationary cycling exercise improved gait abilities in chronic stroke patients. It also concluded that “cycling training stimulates motor regions in the central nervous system and activates the cerebral cortex which eventually improves motor learning and balance.” This has proven true for Sandy, one of my students, who learned ways to keep her balance in check and pick herself up off the ground when she falls. That is, until COVID-19 hit and she wasn’t able to go to her regular exercise classes for three months.
 COVID-19 disrupted the lives of so many people in so many different ways. However, the Michael J. Fox Foundation’s study titled “The Effect of the COVID-19 Pandemic on People with Parkinson’s Disease Study” conducted April 23 through May 23, 2020, revealed crucial information in regards to the Parkinson’s community. “Of the 5,429 people with Parkinson’s in the study, 51 people had the COVID-19 virus. Parkinson’s patients who had COVID-19 reported new or worsening motor and non-motor symptoms. The survey revealed that during a COVID-19 infection, 63% of people with Parkinson’s reported worsening of an existing motor symptom (i.e. tremor, slowness, imbalance) and more than 75% reported worsening of non-motor symptoms (i.e. mood issues, digestive problems, pain and fatigue).”
COVID-19 disrupted the lives of so many people in so many different ways. However, the Michael J. Fox Foundation’s study titled “The Effect of the COVID-19 Pandemic on People with Parkinson’s Disease Study” conducted April 23 through May 23, 2020, revealed crucial information in regards to the Parkinson’s community. “Of the 5,429 people with Parkinson’s in the study, 51 people had the COVID-19 virus. Parkinson’s patients who had COVID-19 reported new or worsening motor and non-motor symptoms. The survey revealed that during a COVID-19 infection, 63% of people with Parkinson’s reported worsening of an existing motor symptom (i.e. tremor, slowness, imbalance) and more than 75% reported worsening of non-motor symptoms (i.e. mood issues, digestive problems, pain and fatigue).”
What was even more remarkable is the number of people with Parkinson’s who didn’t catch the COVID-19 virus but who nonetheless suffered greatly from the experience of the pandemic. “People with Parkinson’s not diagnosed with COVID-19 reported disrupted medical care (64%), exercise (21%), and social activities (57%). . . People with Parkinson’s not diagnosed with COVID-19 reported worsened motor (43%) and non-motor (52%) symptoms.”
The fact that people with Parkinson’s who didn’t catch the virus were affected symptom-wise almost as much as those who did get infected with the virus is quite staggering. And this has held true for my neuro cyclists. None of them have had the COVID-19 virus, but they all experienced worsening of motor and non-motor symptoms and/or new symptoms during the initial COVID lockdown. And in the time since then, it has been an uphill struggle to regain solid ground to get those symptoms back under control.
“The first ride back after missing classes for three months due to COVID-19 was brutal,” commented Bill Brown, Genesis Neuro Cycle Rider, “and walking two miles a day didn’t even begin to cut it for keeping my symptoms at bay. I will say that when I first stopped Neuro Cycling class I felt the benefits from FE classes for about four weeks. But then it dropped fast. Without FE cycling, I began to notice my balance getting rapidly worse. And I had gotten to such a great place cycling pre-COVID. I was hitting up to 90 rpm on my metric assessment rides with my watts up in the 130 range. Coming back, it was 50 rpm, and the watts were so low. I lost so much ground in a very short time. And it’s been extremely difficult building back up.”
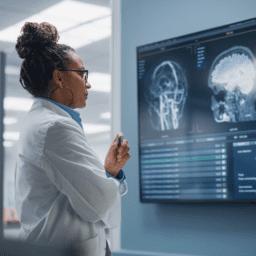
Dr. Alberts recognizes the difficult road that people with Parkinson’s will experience as they navigate their way back to exercising intensely enough to keep their symptoms in check.
“The pandemic disrupted life as we know it. We have to continue to improvise, adapt, and overcome as we move through these times. People with Parkinson’s are accustomed to this, and I have every confidence they can do it,” Dr. Albert said. “It takes time to come back to previous fitness levels after being off or having decreased training for a number of months. The key is coming back safely and progressively. Assuming you have safe access, your new goal should be to reach your pre-COVID fitness level over the next two to four months through careful progression. Having the expectation that you can pick up where you left off will leave you disappointed and likely sore. Nobody sprints up Mt. Everest; they consistently put one foot in front of the other.”
A recent 2020 commentary paper titled, “The Impact of the COVID-19 Pandemic on Parkinson’s Disease” by Rick C. Helmich and Bastiaan R. Bloem, both of whom are experts in the field of Parkinson’s and movement disorders, goes into great depth about what the effects of this pandemic will have on people with Parkinson’s into the future. In this paper they write, “Another hidden but potentially highly disconcerting consequence of the pandemic is a marked reduction in physical activities . . . evidence has shown that physical exercise may attenuate clinical symptom progression in [Parkinson’s.] Nevertheless, a loss of aerobic exercise during the COVID-19 pandemic may well lead to a worsening of motor symptoms in Parkinson’s . . . Furthermore, reduced physical exercise may contribute to increased psychological stress, thereby further aggravating the symptoms of [Parkinson’s].”
“Covid-19 certainly impacted my health, without catching the virus. Previously, I attended five to 11 neuro wellness classes per week. When gyms closed down, I took a short time off myself, but I knew that was risky. When I started exercising at home, I had lost both muscle and stamina,” said Jane Collison, Genesis Neuro Cycle rider. “For me, with loss of strength goes balance. Cycling has been my exercise of choice to combat Parkinson symptoms. I started cycling as soon as I was diagnosed. Through consistent workouts, I became strong. I went from 48 watts to 100 watts. And, from 60 RPM to easily hitting 94 RPM. Upon coming back from the three month’s away from ‘FE,’ the decline in my biking abilities was very noticeable. However, I will climb my way back because I know my symptoms are better when I cycle.”
Parkinson’s is a chronic, progressive, degenerative condition mostly seen after the age of 50. There is treatment, but no cure. Parts of the brain in people with Parkinson’s produces insufficient amounts of dopamine. Dopamine transmits information from the brain to our muscles, allowing them to move. So forced pedaling causing more messages to the brain changes the brain by activating the same areas that medication would activate. Cycling also increases the connectivity in the brain’s gray matter, which can subsequently help lessen the symptoms of Parkinson’s.
 Another study by Dr. Alberts titled, “The Effect of Forced-Exercise Therapy for Parkinson’s Disease on Motor Cortex Functional Connectivity” looked at how FE and medicine produce similar changes in brain activation patterns in people with Parkinson’s. In fact, the study proved that “FE improved [participants’] motor functions clinical ratings by 51% compared to 33% in those who received medication.”
Another study by Dr. Alberts titled, “The Effect of Forced-Exercise Therapy for Parkinson’s Disease on Motor Cortex Functional Connectivity” looked at how FE and medicine produce similar changes in brain activation patterns in people with Parkinson’s. In fact, the study proved that “FE improved [participants’] motor functions clinical ratings by 51% compared to 33% in those who received medication.”
The research showed how the effect of the blood flow in the brain affected brain function after the work out. “Exercise has a strong effect on baseline cerebral blood flow, with increases in the motor cortex of up to 20% up to 30 min after exercise (Smith et al., 2010). Concomitant changes in physiology (systolic and mean arterial blood pressure) showed evidence of normalization by 30 min after. It is unknown whether these cerebral blood flow changes persist after [one or two hours] following exercise.”
Sandy Trent says she definitely gets a huge benefit from increased blood flow to the brain resulting in increased cerebral function after neuro cycling. In fact, the first time she experienced it was four years ago, after her first indoor cycle class. She went 62 years without experiencing mental clarity after her stroke. Now, she experiences mental clarity for three to four hours following each cycle class.
Cycling can have a positive impact on anyone affected by disease. A 2015 study conducted in the Netherlands had scientists analyzing the effects of physical activity on the brain. They randomly assigned healthy patients and schizophrenic patients to a six-month exercise program on stationary bikes. Brain scans of subjects assigned showed a significant increasing the strength of white matter fiber in both healthy and schizophrenic patients.
The brain is made up of two kinds of tissues: grey matter, which has all the synapses and is the command center of your body, and white matter, which is the communication hub, using axons to connect the different parts of grey matter. The more white matter you have, the faster you can make important connections. So, anything that increases white matter is good and cycling does exactly that. It improves both the integrity and density of white matter and speeds up connections in the brain.
But, it doesn’t stop there. Cycling also fires up extra nerve cells, intensifying the creation of a protein called brain-derived neurotrophic factor (BDNF) — a protein that helps maintain existing neurons and create new ones. A 2015 study, conducted at Taichung Veterans General Hospital in Taiwan, found that after cycling for 12 weeks, participants increased lower extremity muscle strength and showed a spike in BDNF. BDNF is also responsible for regulating stress, mood, and memory. This might explain previous research that has found cycling to be associated with lower levels of depression and anxiety. All helpful things for people managing neurological disease.
 Cycling also increases blood levels of a natural cannabinoid called anandamide. Cannabinoids are the ones that act like marijuana, which explains why so many people feel a “cyclist’s high” during a long ride. When the endocannabinoid system is activated, it gives cyclists a boost of euphoria, enhances creative thinking, and helps riders find solutions to problems.
Cycling also increases blood levels of a natural cannabinoid called anandamide. Cannabinoids are the ones that act like marijuana, which explains why so many people feel a “cyclist’s high” during a long ride. When the endocannabinoid system is activated, it gives cyclists a boost of euphoria, enhances creative thinking, and helps riders find solutions to problems.
Citations and more research available on the PDF of the article here.
About Kris Meldrum
Parkinson’s Wellness Coach Kris Meldrum has more than 15 years in the fitness industry and worked a decade in the Medical Fitness Industry before starting Genesis Health Club’s Neuro Wellness Program in 2020. She has published several Parkinson’s/neurological articles that she vets through Jay Alberts, PhD, Vice-Chair of Innovation in the Neurological Institute and Neuroscientist in The Cleveland Clinic Lerner Research Institute. Kris is an ACE Senior Fitness Specialist; an ACE Certified Group Fitness Instructor; an ACE Approved Parkinson’s Cycle Coach; a Certified Madd Dog SPINNING Advanced Instructor; Madd Dog SpinPOWER Instructor; a Certified Rock Steady Boxing Parkinson’s Head Coach & Trainer; a Certified Parkinson’s Delay the Disease Instructor, and has completed the APDA Parkinson’s Training for Fitness Professionals. Kris also speaks at Parkinson’s Conferences about “The Science and Methodologies of Parkinson’s Exercise—How to Exercise to Improve Symptoms.”