About 10-20% of people diagnosed with Parkinson’s are labeled as having Young Onset Parkinson’s disease (YOPD). Recently, The Task Force on Early Onset Parkinson’s Disease (EOPD), led by Dr. Rodolfo Savica, sought to create a definition of (EOPD/YOPD) to align the medical community. Based on their work, they came up with age 55. That said, it’s more complicated than picking one number. In this interview, Melani Dizon, Director of Content and Education at the Davis Phinney Foundation, asks Dr. Savica about the age cut-off, naming conventions, the difference between early- and late-onset Parkinson’s, and much more.
You can read the transcript below or you can Rodolfo Savica YOPD Transcript
Note: This is not a flawless, word-for-word transcript, but it’s close.
Why is it important to address yopd as eopd?
The main reason why the Task Force suggested changing the name of YOPD to EOPD is that the word “young” does not describe what is happening in a person’s body. The distinction between early-onset Parkinson’s and late-onset Parkinson’s (LOPD) is that EOPD appears without the presence of aging factors. For example, someone with LOPD will have plaques present that are similar to those of dementia and other diseases that are associated with aging. They are probably getting Parkinson’s because their brain is aging, and the basal ganglia are having more issues producing dopamine. On the flip side, people who get Parkinson’s earlier in life develop it due to external factors, such as pesticides or brain trauma. The International Parkinson and Movement Disorder Society Task Force on Early Onset Parkinson’s Disease describes it as such:
Authors who have first developed an interest in, and published on, this subgroup of PD have preferred the use of YOPD. However, there has been a shift toward the use of EOPD in the past 2 decades. There are no clear publications detailing the rationale behind this shift, but it seems motivated by an attempt to avoid age-related stigmatization (Table 1). Thus, the recommendation of the Early Onset Parkinson Disease Task Force of the MDS is to use the term EOPD to be designated with an onset of motor symptoms before the specific age that was agreed on.
You can read their full paper here.
The Task Force did not come to this decision easily, but the main purpose of it is to define the difference between EOPD and LOPD medically so doctors can better treat their patients. Many in our community feel strongly about using the term YOPD, and we have decided to continue using that term. The paper’s main point is that there needs to be an international consensus on the distinction and definition within the medical community so that they can provide the best care possible no matter where their patients live.
What are the main differences between Yopd and lopd?
Here are some key differences:
- People with LOPD have similar symptoms, while people with YOPD have varying symptoms. This is also why it is easier to get diagnosed with LOPD when initially presenting symptoms, while people with YOPD are typically diagnosed years after first presenting symptoms.
- Dopamine production is altered in both YOPD and LOPD. However, people with YOPD are dealing with their brains suddenly deteriorating, while people with LOPD have signs of aging that Parkinson’s exacerbates.
- In females, having YOPD can cause extreme fluctuations in the presentation of symptoms. During menstruation, women experience more intense OFF periods due to blood loss. Women with LOPD have usually already gone through menopause and therefore experience OFF periods equivalent to those of their male counterparts. This distinction is directly related to people with the XX chromosome, not based on gender expression. However, it is important to make this distinction as studies on women with Parkinson’s, particularly women with YOPD, are rare. Women will take longer to address their symptoms than their male counterparts, and since there is less research on women with Parkinson’s, they are less likely to be diagnosed.
- In people with LOPD, the first symptom to show itself is usually dyskinesia. In people with YOPD, the symptom that presents itself first is typically dystonia.
- The prognosis for people with LOPD is living another 12 to 14 years after diagnosis. They will typically pass away due to other factors related to aging, such as cancer or cardiovascular issues. For people with YOPD, the prognosis is living another 48 years after diagnosis. However, they will most likely pass away due to similar factors.
How can DISTINGUISHing between the two help with treating parkinson’s?
When we understand that YOPD and LOPD are two different diseases, we can better understand what a person needs to live their best life. For example, while people with LOPD may want to try Rock Steady Boxing or an activity similar to that, people with YOPD can often continue exercising with their non-Parkinson’s peers of a similar age and at a similar level.
Some people diagnosed with YOPD choose to get a DaTscan to either confirm their diagnosis and/or see if something else is happening, such as essential tremor or drug-induced Parkinsonism.
Finally, while people with LOPD can get Deep Brain Stimulation (DBS) surgery, people with YOPD are encouraged to get it earlier as it can improve their quality of life and slow down the progression of their symptoms. It is not necessary to get DBS or the right fit for everyone; however, for some, it can give them their life back.
Thank you so much, Dr. Savica, for informing us about your work with the International Movement Disorder Society task force and early onset Parkinson’s. Email blog@dpf.org if you have questions.
 JOIN OUR PELOTON CLUB
JOIN OUR PELOTON CLUB
Our educational content is made possible because of the monthly donors in our Peloton Club. Want to become a member and help us continue to create the resources people need to live well with Parkinson’s? Learn more and register to become a member here. (You’ll get a cool gift if you do!) It’s as easy as can be to set it and forget it.
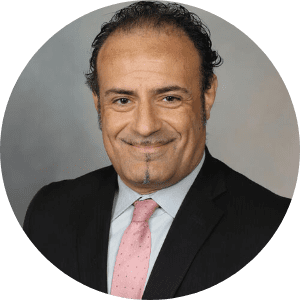
Meet the speaker: Rodolfo savica, md
Rodolfo Savica, MD, PhD, studies the early-life predictors of neurodegeneration and the mechanisms that lead to neurodegenerative disorders such as Parkinson’s, dementia, and Lewy body dementia. Dr. Savica is a Professor of Neurology of Practicing Neurologists and Movement Disorder and Behavior Specialist at the Mayo Clinic in Rochester, Minnesota. He has a particular interest in early-onset Parkinson’s and initiatives regarding the clinical practice and research of early onset and is the chair of the International Movement Disorder Society Task Force on early-onset Parkinson’s. Dr. Savica also leads a lab to find a cure and improve the quality of life for people with Parkinson’s.
Thank You to Our 2023 Live Well Today Webinar Series Presenting Sponsors
*While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.