Written by Kris Meldrum, BA ACE, Neuro Wellness Program Lead, Neuro Wellness Parkinson’s Coach
Vetted by Dr. Jay Alberts, PhD, Vice-Chair of Innovation in the Neurological Institute and Neuroscientist, Cleveland Clinic
(Note: This article, in two parts, was originally published in the 2020 Winter Rock Steady Boxing In Your Corner Magazine. We received permission from the author to publish here with minor edits to improve readability on our blog.)
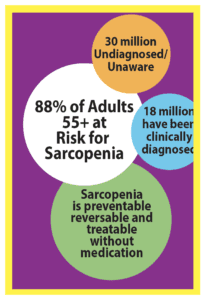
88% of Adults 55+ at Risk for Sarcopenia, 1-in-5 PD Patients Have Severe Case
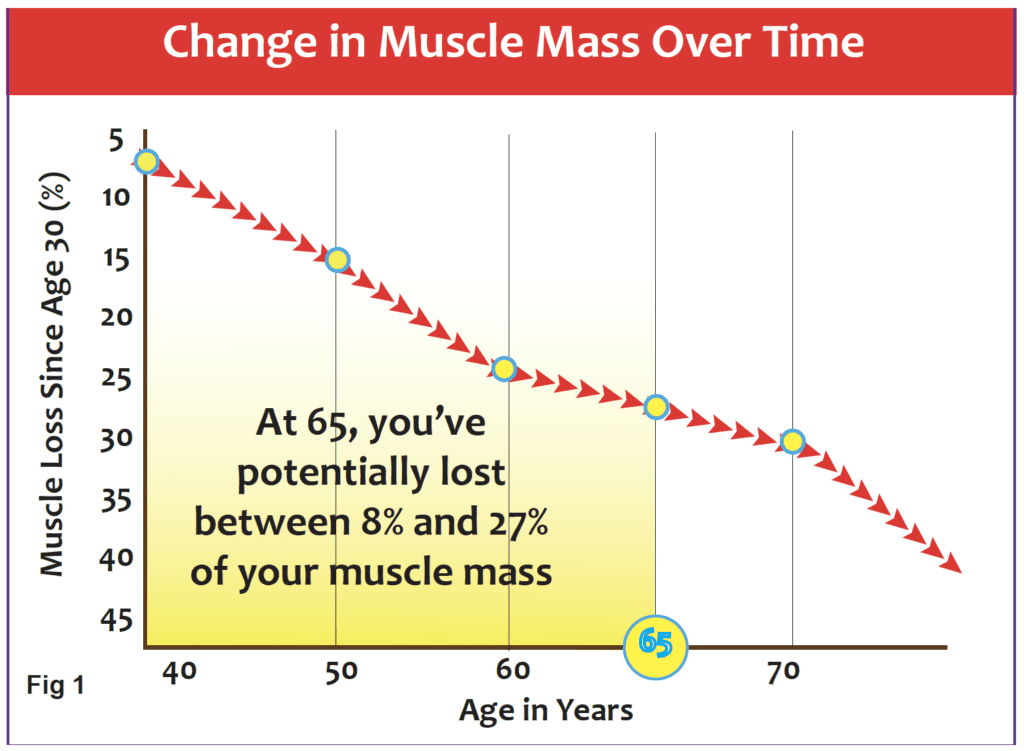
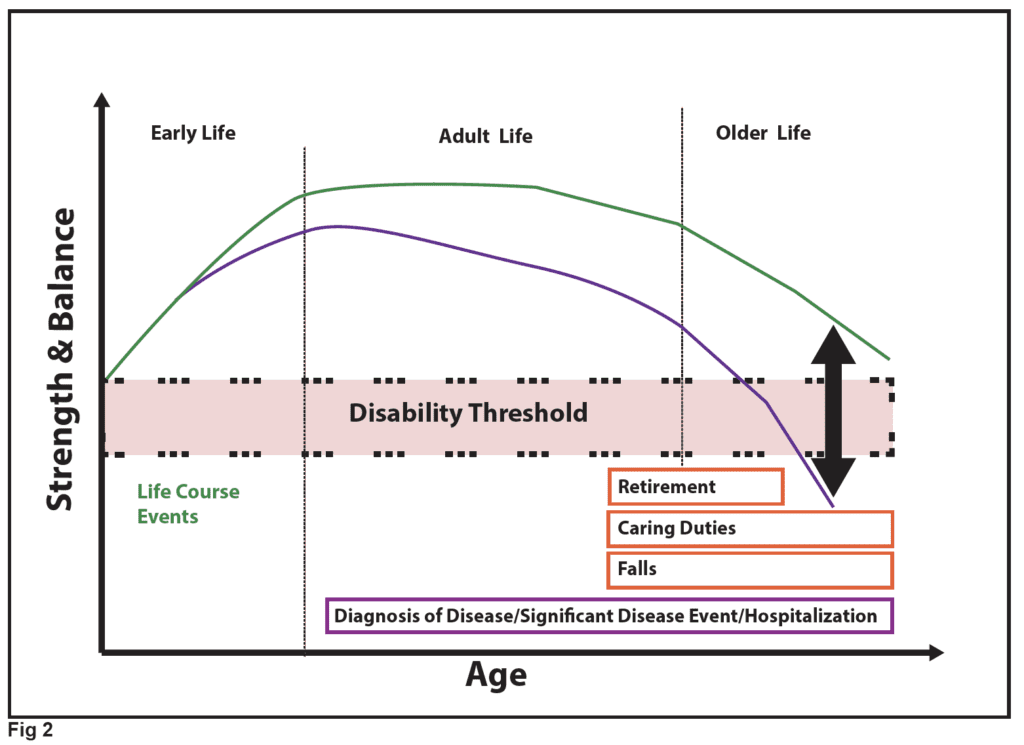
We have all heard the phrase “use it or lose it.” Well, when it comes to muscle mass, this mantra is very true. Working the muscles as we age helps maintain muscle mass and strength. When muscles are not used, they shrink. It’s as simple as that. Unfortunately, power ebbs at an even faster rate than strength. And, while strength is important, the ability to generate power has a greater impact on a person’s ability to perform the activities of daily life—swinging a bag of groceries to the counter, going up the stairs to grab something quickly, or running across the crosswalk because the light suddenly turned yellow. What isn’t stressed enough in our culture is that from the age of 40 on, we significantly start to lose muscle mass, function, and strength in the body—a condition associated with the aging process called sarcopenia. Why is this important? Because this change with age over time can affect balance, gait, and a person’s overall ability to perform simple tasks of daily living. Why is it even more important for people with neurological diseases? Because it’s a double whammy for them. One, they have to fight the effects of sarcopenia, and two, on top of that, they have to fight the myriad of symptoms associated with their disease.
 What is the impact of sarcopenia on people with neurological diseases? According to the various research studies and scientists currently evaluating its effects, sarcopenia is quite different for Parkinson’s, Alzheimer’s, stroke, etc. However, this article will focus on Parkinson’s disease (PD). In one research study with 210 PD patients, sarcopenia was found to be very common among PD patients, and 1 in 5 were diagnosed with severe sarcopenia. “The prevalence of sarcopenia was 28.5%-40.7% in men and 17.5%-32.5% in women. The prevalence of severe sarcopenia was 16.8%-20.0% in men and 11.3%-18.8% in women.”
What is the impact of sarcopenia on people with neurological diseases? According to the various research studies and scientists currently evaluating its effects, sarcopenia is quite different for Parkinson’s, Alzheimer’s, stroke, etc. However, this article will focus on Parkinson’s disease (PD). In one research study with 210 PD patients, sarcopenia was found to be very common among PD patients, and 1 in 5 were diagnosed with severe sarcopenia. “The prevalence of sarcopenia was 28.5%-40.7% in men and 17.5%-32.5% in women. The prevalence of severe sarcopenia was 16.8%-20.0% in men and 11.3%-18.8% in women.”
Not only is sarcopenia prevalent in Parkinson’s patients, but there seems to be a link between the pathways that both diseases use because neurodegeneration is a part of the onset of sarcopenia. A study by J.N, Caviness studied hand muscle measuring and found, “There is some evidence that at least a proportion of PD and sarcopenia patients share a common pathway of dopaminergic dysfunction and reduced numbers of motor neurons . . . they found significantly lower motor unit numbers in the hand muscles of PD patients compared to healthy controls using different MUNE (Motor unit number estimation) techniques, a measure that is comparable to MUNIX (Caviness et al., 2002). In summary, these findings suggest that a common pathway exists at least in subpopulations of both diseases.”
Another study held in Brazil evaluated 218 PD patients and the correlation between sarcopenia and falls in PD patients. In its published findings in March of 2020, it said, “Falls in PD involve very complex multifactorial mechanisms and recurrent falls is a milestone of disease progression [32]. Falls were significantly more frequent in patients who were screened positive in the SARC-F (those with sarcopenia) compared to those screened negative. . . Several studies have shown that reduced mobility, poor balance, and reduced leg muscle strength have been associated with increased fall risk [30–31]. These signs are clinical manifestations of sarcopenia.”
What researchers concluded is that it’s important to assess PD patients for sarcopenia—check their body composition, mass, and muscle strength assessment. “Sarcopenia and PD share common pathways and, regardless of their source, they may affect each other’s prognosis and patients’ quality of life.” This study found that early diagnosis, prevention, and intervention for sarcopenia could decrease functional decline in patients with PD. This study also stated, “Adding a high protein diet and resistance exercise training could help reverse or improve this condition. The sooner these interventions are implemented, the more likely PD patients will benefit from them.”
These recommended components are ones that anyone can use to reverse the effects of sarcopenia, along with adding measures such as increasing vitamin D and amino acids, according to researchers. “Nutrition and especially amino acid intake are important to maintain protein turnover, but what amounts and types are optimal remain to be determined. Vitamin D plays a relevant role in muscle function. Exercise is beneficial and will decrease body fat, improve reserve capacity, and increase muscle strength.”
Scientists originally said sarcopenia was an inevitable process that happens to everyone over time; however, there are now specific points where a person loses enough muscle mass to cross a threshold for sarcopenia to be classified as a disease. According to Taylor J. Marcell’s research article, Sarcopenia: Causes, Consequences, and Preventions, “A clear relationship exists between loss of muscle strength and loss of independence, contributing to falls, fractures, and nursing home admissions . . . what is the minimal amount of muscle mass and strength required to maintain independent living with advancing age?”
According to J. Morely’s article, Sarcopenia: Diagnosis and Treatment, “a loss of 30% of reserve capacity limits normal function, whereas a decrease of 70% results in failure of that system. Sarcopenia is evident in approximately 20% of individuals over 70 years old; this figure rises to 50% in the over-80 age group.
The National Strength and Conditioning Association (NSCA) released its position on resistance training for older adults in October of 2019. The abstract summary stated, “Current research has demonstrated that countering muscle disuse through resistance training is a powerful intervention to combat muscle strength loss, muscle mass loss (sarcopenia), physiological vulnerability (frailty), and their debilitating consequences on physical functioning, mobility, independence, chronic disease management, psychological well-being, and quality of life.” The statement documents 11 summary statements for effective resistance training regarding older adults. And, the list does include those people who have neurological diseases, as well as people who are living in nursing homes. A goal of the NSCA is to break down the fear and barriers that older adults have of resistance training. “More than 80% of adults do not meet the guidelines for both aerobic and muscle-strengthening activities.” It’s vital to help them understand why it’s so important to their quality of life as they age.
 The NSCA Position Statement detailed that an older adult’s exercise program should include a combination of strength, power, and endurance in order to counteract declines in muscular strength, mass, cardiorespiratory fitness, neuromuscular function, and functional capacity.
The NSCA Position Statement detailed that an older adult’s exercise program should include a combination of strength, power, and endurance in order to counteract declines in muscular strength, mass, cardiorespiratory fitness, neuromuscular function, and functional capacity.
A big emphasis is on power training (NOT powerlifting) that involves performing concentric actions explosively up to maximal exertion. Muscle power has been shown to promote greater functional improvement in a person’s ability to perform daily activities. “Incorporating power exercises—performed at 40%–60% of 1-RM—is also encouraged in resistance training program design for seniors.” So, for instance, a person would perform a squat with three slower counts down, and then “power up” with more speed, on the one up count. Or, if they were doing a bicep curl, they would go down three counts slowly, and again, “power up,” with more speed, on the one up count. And, of course, all programs should have a balance among training variables (volume, intensity, frequency, exercise selection, exercise order) and workout duration for both aerobic and resistance training.

The study took into account not just healthy adults, but noted that resistance training programs could be modified to benefit older adults with frailty, mobility limitations, cognitive impairment, or other chronic conditions. It went on to state, “Resistance exercise results in favorable neuromuscular adaptations in both healthy older adults and those with chronic conditions. These adaptations translate to functional improvements of daily living activities, especially when power training exercise is included. In addition, resistance training may improve balance, preserve bone density, independence, and vitality, reduce risk of numerous chronic diseases. . . . Both research and clinical experience indicate that resistance training is safe for healthy older adults (404), frail (physiologically vulnerable) older adults (94,621), and individuals with disease.”
Part Two – Programs designed to help with these issues
Neuro Cycle
The Neuro Cycle Program provides a monitored and safe exercise protocol for all participants. The rider can pedal in a controlled environment while being observed as well as coached properly. The first periodization of training focuses on “forced exercise”—defined as exercising beyond a voluntary level with a goal to get the rider at a cadence of 80 rpm. The more pedal strokes per minute cause more muscle contractions, which send more nervous system messages to the brain. Researchers have shown that biochemical reactions are the result of these messages. Consequently, the more messages the brain receives, the greater the response resulting in better motor function. “New studies of the effects of forced exercise in Parkinson’s patients found that forced exercise improved patient’s motor functions clinical ratings by 51% compared to 33% in patients who received medication.” The symptoms that were improved were tremors and upper body motor control. The lessening of symptoms was sometimes maintained as long as four weeks after the riders stopped. This improvement of upper body motor control is significant in that it helps enable better functionality for a PD patient to be able to incorporate resistance training in other classes to help combat sarcopenia.
Sarcopenia affects the lower body muscle mass more than the upper body. “Muscle mass and strength of the lower body is affected to a greater extent by age than is the upper body, most likely because a reduction in physical activity (i.e.., walking, running) would have a greater effect on the lower body (4,6–9). Moreover, individuals with weak lower limbs tend to supplement lower body movements with other muscles (such as arm muscles) to help rise from a chair or alter their behavior to avoid activities such as climbing stairs (10).”
Cycling gives an individual the opportunity to build the muscles of the lower leg in a safe way. As the quadriceps, hamstrings, and calves become stronger through cycling, everyday activities become easier to handle. Also, exercise is considered an essential part of therapeutic strategies to target age-related sarcopenia, and Harber et al. (2012) reported that cycle exercise increased muscle size and strength in both 20-year-old and 74-year-old subjects.
Rock Steady Boxing
Rock Steady Boxing (RSB) was founded in 2006 by former Marion County (Indiana) Prosecutor Scott C. Newman, who is living with Parkinson’s. The goal of RSB is to educate as many people as possible about the benefits of intense exercise and to establish safe and welcoming programs in every community for people with Parkinson’s to fight back against their disease.
RSB, like cycling, focuses on “forced exercise” defined by M.A. Hirch’s research as“the importance of exercise intensity in PD suggest that PD patients without specific contraindications should be encouraged to begin exercise training programs that focus on achieving a higher training intensity, beyond what they may self-select.”
RSB is a non-combat functional training program that incorporates activities for the whole body. The boxing training program starts with a 20-minute warm-up of breathing, get-to-know-ya’s, chants, songs, and stretching exercises for major muscle groups. The warm-up is followed by a 45-to-60-minute circuit training regimen of functional fitness, endurance calisthenics, such as push-ups, skipping, and jumping rope, along with boxing ring work, which focuses on footwork and agility drills.
RSB is jam-packed with strength, power, balance, and endurance components to its workout—which is why it is such an effective program, not only physically, but emotionally. The punching activities include punching heavy bags, speed bags, and focus mitts—padded mitts worn by an RSB Coach to prompt the practice of various combinations of punches toward moving targets. Boxers are treated as athletes and encouraged to train as intensely as they can and achieve more than they think is possible. The session ends with a 15-to 20-minute cool-down that emphasizes core stretching, strengthening, and breathing exercises.
RSB also has special components to its workout, like fall prevention, where boxers are taught how to fall in a safe manner which helps them overcome their fear of falling, so they can participate more fully in life. Boxers train to improve their balance, hand-eye coordination, speed of movement, agility, muscle, power, mental focus, and rhythm.
In a Case Series Observational Study of Rock Steady Boxing, researchers found that “all patients showed improvements in every outcome category, including balance, gait, disability, and quality of life. These positive changes may be indicative of the whole-body approach of the boxing training program . . . Another key observation of this case series was that all patients continued to make improvements in balance, gait, and quality of life up to the 24-and 36-week tests despite the reduction in attendance after the initial 12 weeks. The majority of changes that achieved and surpassed the established minimal detectable change (MDC values) were seen at the 36-week test.”
The Rock Steady Boxing workouts contain all the building blocks, to not only fight back against Parkinson’s, but also sarcopenia. It also has the flexibility within its model to add the recommended NSCA resistance training variables for older adults:
- 2 multi-joint exercises per major muscle group, achieving intensities of 70–85% of 1 repetition maximum (1RM)
- Power exercises performed at higher velocities in concentric movements with moderate intensities (i.e.,40–60% of 1RM)
“Rock Steady Boxing (RSB) is about empowering people with Parkinson’s around the world to fight back against their disease. We accomplish this through community-based franchise programs—like RSB Genesis Health Club WDM, who are not only bringing RSB to Midwest PD patients, to help slow the progression of their disease and build comradery in their community, but they have brought together a whole suite of PD programs at an affordable cost. And this is exactly the vision that RSB founder Scott C. Newman had when he started RSB. Scott wanted the program available to as many PD patients as possible and as affordable as possible. Putting people first is the heart of RSB.”
– Kristy Rose Follmar, CPT, HQ, IN, RSB Program Director/Head Coach
Delay the Disease
The OhioHealth Delay the Disease™ (DTD) class is a Parkinson’s-specific exercise program that helps students learn to take control of their symptoms. DTD creates an environment that promotes support, community and comradery. Each class includes brief episodes of high-intensity aerobic work followed by PD-specific task training–core stability, strength training, dual-task training, large-amplitude walking, rotational movements, integrated cognitive challenges, fine motor drills, and balance training which are incorporated at a challenging level of difficulty for all functional abilities. In fact, levels of difficulty for the exercises are modified for students into Level A (basic) Level B (a bit tougher), and Level C (the hardest). DTD is an evidence-based fitness program, launched in 2005 by co-founders Jackie Russell and David Zid, designed to empower people with Parkinson’s disease and other neurological disorders, as well as their caregivers and spouses.
“We have helped tens of thousands of people with Parkinson’s regain control, improve strength, mobility, balance and minimize depression. We utilize eccentric strength training in all functional levels of our classes, including chair-based programs. It is never too late to start exercising in the course of this disease, and certainly never too early.”
– Jackie Russell, RN, BSN, CNOR, Co-Founder OhioHealth Delay the Disease and David Zid, BA, ACE, APG, Co-Founder OhioHealth Delay the Disease
Due to its comprehensive and encompassing nature, DTD classes have everything within their scope to combat sarcopenia—cardio, resistance training, balance training, stretching, etc. Like the RSB program, DTD also has special focus areas to address real-life situations that PD patients face, like falling and getting up after a fall. The classes specifically train students how to get up from the floor independently and teach functional balance moves and the use of a wide-based gait to improve stability. A recent three-year retrospective review of DTD outcomes demonstrated clinically significant improvement in fall risk, quality of life, depression, and functional mobility. (In submission for publication) “Exercise programmes that are ongoing and that include balance challenging exercises are effective as a single intervention in preventing falls.”
Tai Chi
And to round out a well-balanced Neuro Program, the tai chi class is an effective therapy for PD Patients, because it improves a person’s balance, ability to walk, and move steadily. Research has shown that tai chi can reduce the chances of falls, build muscular strength (which is important to help combat sarcopenia), improve mobility and coordination, and help focus the mind. “Tai chi can be highly effective for preventing falls. Tai chi is a safe and accessible form of exercise. Indeed, over 500 trials and 120 systematic reviews have been conducted on the health benefits of tai chi.”
In a research study in China, PD participants were divided into two different groups to perform routine exercises including treadmill training, aerobic training, and tai chi for three consecutive days, over a period of two months. “500 patients with confirmed Parkinson’s disease (severity level I to III) were collected and analyzed. Participants who received 80 min/day tai chi 3 times/week for 2 months were included in the tai chi (TC) group (n=250) and those who received 90 min/day routine exercise 3 times/week for 2 months were included in routine exercise (RE) group (n=250).”
At the end of the two months, everyone felt good about their exercise program—found exercise movements easy, safe, and appropriate. Most of all, the exercises helped them improve their confidence and balance. However, nine percent of the patients were successful in getting off levodopa or equivalent medication. Also, the tai chi group saw a decrease in the daily dose of levodopa or equivalent medication. “The efficacy of tai chi specifically in the case of PD is explained by its role in normalizing the levels of neurotransmitters including dopamine and acetylcholine in various regions of the brain, i.e., cortex, basal ganglia, and motor cortex feedback loop. When tai chi is practiced daily, it promotes the development of various de novo neural pathways in a PD patient that results in a fast response to posture challenges (10). Tai chi exercise delayed the introduction of levodopa.”
Although aging is part of every person’s daily life, developing sarcopenia does not have to be. Fortunately, there are steps people can take that decrease their chances of losing significant muscle mass. And, even if muscle mass has been lost, it can be regained with proper diet, resistance, and cardio training. Each person should work with a doctor to find out what key nutrients, supplements, hormones, and foods, along with a comprehensive exercise plan, works for them. It is all about keeping everything balanced and moving forward in the right direction.
 Parkinson’s Wellness Coach Kris Meldrum has more than 15 years in the fitness industry and worked a decade in the Medical Fitness Industry before starting Genesis Health Club’s Neuro Wellness Program in 2020. She has published several Parkinson’s/neurological articles that she vets through Jay Alberts, PhD, Vice-Chair of Innovation in the Neurological Institute and Neuroscientist in The Cleveland Clinic Lerner Research Institute. Kris is an ACE Senior Fitness Specialist; an ACE Certified Group Fitness Instructor; an ACE Approved Parkinson’s Cycle Coach; a Certified Madd Dog SPINNING Advanced Instructor; Madd Dog SpinPOWER Instructor; a Certified Rock Steady Boxing Parkinson’s Head Coach & Trainer; a Certified Parkinson’s Delay the Disease Instructor, and has completed the APDA Parkinson’s Training for Fitness Professionals. Kris also speaks at Parkinson’s Conferences about “The Science and Methodologies of Parkinson’s Exercise—How to Exercise to Improve Symptoms.”
Parkinson’s Wellness Coach Kris Meldrum has more than 15 years in the fitness industry and worked a decade in the Medical Fitness Industry before starting Genesis Health Club’s Neuro Wellness Program in 2020. She has published several Parkinson’s/neurological articles that she vets through Jay Alberts, PhD, Vice-Chair of Innovation in the Neurological Institute and Neuroscientist in The Cleveland Clinic Lerner Research Institute. Kris is an ACE Senior Fitness Specialist; an ACE Certified Group Fitness Instructor; an ACE Approved Parkinson’s Cycle Coach; a Certified Madd Dog SPINNING Advanced Instructor; Madd Dog SpinPOWER Instructor; a Certified Rock Steady Boxing Parkinson’s Head Coach & Trainer; a Certified Parkinson’s Delay the Disease Instructor, and has completed the APDA Parkinson’s Training for Fitness Professionals. Kris also speaks at Parkinson’s Conferences about “The Science and Methodologies of Parkinson’s Exercise—How to Exercise to Improve Symptoms.”
Learn More
What You Need to Know about Osteoporosis and Parkinson’s
How Sunlight Can Help You Live Well with Parkinson’s
The Latest and Greatest on Boxing and Parkinson’s