Deep brain stimulation (DBS) is a highly effective and reasonably safe treatment for Parkinson’s; however, it’s also frequently misunderstood. The success stories about how people are sometimes living symptom and medication-free as a result of getting DBS understandably lead many to want to get the treatment as soon as possible. Others think it sounds scary and shy away from it.
In this episode
Dr. Joohi Jimenez-Shahed broke down the what, why, and how of DBS and its latest advancements.
To download the transcript, click here.
Show Notes
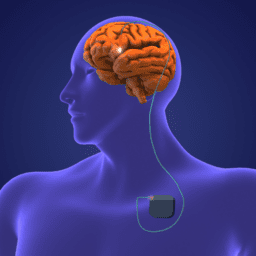
What is DBS and how does it work? DBS stands for deep brain stimulation, a surgical therapy during which a battery and wires are placed in the brain, with electrodes placed on areas in the brain that are responsible for movement. After the surgery, the device is activated and programmed over a period of four to six months. The device sends electrical impulses to these motor areas to correct for this circuitry not firing correctly on its own in Parkinson’s.
How does someone know they’re ready for DBS? It depends on the individual, but DBS is often recommended for people who meet certain requirements when medications are no longer managing OFF times effectively or there is a high occurrence of tremor, dyskinesia, or dystonia.
Who is the ideal candidate for DBS? In general, the criteria for receiving DBS are the following:
-
- The person’s symptoms should be responsive to levodopa. This is typically the case in idiopathic Parkinson’s, but is not always the case in Parkinsonism, essential tremor, or Atypical Parkinson’s. If your symptoms do not respond to levodopa, they will not respond to deep brain stimulation.
- While experiencing non-motor symptoms such as depression, anxiety, or cognitive difficulties such as memory loss does not rule someone ineligible for DBS, medical professionals may proceed with extra caution in these cases, as there may be a risk of these symptoms worsening after the surgery.
- If someone has many other medical conditions, DBS may or may not be an option, as co-morbid conditions may affect the effectiveness of the device or the safety of the procedure.
Is there an age limit for getting DBS? Although there have been suggestions in the past that people over 70 should not get DBS, medical professionals now primarily look at the above criteria to determine if DBS is a good fit.
Are there any non-motor symptoms that improve with DBS? Although non-motor symptoms may not be directly affected by DBS, the therapy does reduce OFF times, and this may result in fewer non-motor symptoms.
What is the history of DBS? The practice of deep brain stimulation has evolved over time, but all started with an accidental discovery that found that people with Parkinson’s who had also had a stroke in a particular region of the brain had a reduction in their Parkinson’s motor symptoms after undergoing brain stimulation.
What types of DBS devices are available? All DBS devices have the same basic components, but there are slight variations in the “bells and whistles” based on the manufacturer. These differences include extra precise control of electrical impulses, the ability to steer the electrical current in a particular direction, and the ability to sense and record electrical signals. DBS devices may also offer differences in battery type, with some featuring replaceable batteries and others rechargeable batteries.
Who decides which device you get? It may vary from place to place. People undergoing DBS are welcome to voice their preferences, but there may be some limitations as to which device you get based on the facility, the surgeon performing the surgery, and your insurance.
How does someone go about finding and selecting a neurosurgeon to do the surgery? Usually a referral to a surgeon will come from your neurologist, but as a person with Parkinson’s, it is important to feel empowered to ask additional questions to establish confidence in your surgeon. Some questions you may ask are:
-
- How many DBS cases has the surgeon done?
- How familiar is the surgeon with the procedure?
- What is the surgeon’s complication rate and/or rate of side effects?
What are the pros and cons of different types of batteries? The conventional battery life depends on the programming that’s required to control the symptoms. The average life of a conventional battery is three to five years. Rechargeable batteries are currently estimated to last up to 25 years, but rechargeable batteries require regular re-charging approximately once a week.
How long do the non-rechargeable batteries last and what does the process look like to replace the battery? Non-rechargeable batteries tend to need replacing every three to five years. When replacing a battery, you will likely go under general anesthesia, and the surgeon will go in through the same incision used to originally place the battery. The procedure typically lasts about an hour, and most people having the surgery will go home the same day.
What does programming a DBS device look like? When you get DBS, it is not as simple as turning it on. Following the surgery, it typically takes four or five sessions over the course of approximately six months to program your DBS with a specialist.
What are DBS options for individuals who live in more remote areas? Remote programming now exists for certain DBS devices, which allows the user to program their device at home during a virtual visit with their physician. This process does, however, require a good internet connection, which may be a challenge for some people living in rural communities.
What are some of the limitations of the technology? The most important thing to recognize is that DBS is not a replacement for your medications. DBS works in conjunction with your medications to reduce OFF times, reduce dyskinesia, and increase ON times. Parkinson’s will continue to progress, and though increasing stimulations may help to control the progression of these symptoms, DBS does have its limitations.
Is there an advantage to getting DBS earlier in the course of Parkinson’s? In the past, it was suggested that people should only receive DBS as a last resort. This is no longer the case, and in general, the guidelines for receiving DBS are based on a general set of criteria rather than length of time since diagnosis or age.
What are some of the exciting advancements happening in DBS right now? This is an exciting time in the advancement of DBS. Some of the most recent advancement include devices that have remote programming capability, new brain imaging devices, and new devices that can sense and track brain signals, which may be helpful in eventually understanding the brain activity for certain symptoms, and therefore, optimizing treatment.
Is DBS reversible? Yes, DBS devices can be turned off or taken out.
How long does the surgery take? The surgery is usually split into two, sometimes three, procedures. The first procedure involves placing the brain electrodes (sometimes the surgeon will split this into two surgeries, one for each side of the brain). After this procedure, most people will be required to stay overnight to ensure there are no complications. Then, there will be a follow-up procedure to place the battery. This surgery typically involves a general anesthetic, and the people undergoing the procedure is typically in and out of the hospital the same day.
What is the success rate of DBS? Generally, success rates are very high. The expected result is to see the same reduction of symptoms that you once had when your medications were working optimally.
Can you upgrade your DBS system? Swapping out electrodes would likely not be recommended due to the invasiveness of the surgery. If there were to be new advancements in batteries, you may or may not be able to swap this out, based on its compatibility with your primary device.
What is the cost of DBS and is it covered by insurance or Medicare? DBS is considered a standard of care surgery and so is typically a covered surgery, Medicare included. Specific costs will be based on your insurance coverage.
Additional Resources
The What, Why, How, and More of DBS for the Newly Diagnosed
[Webinar Recording] A DBS Forum
Life Before and After Deep Brain Stimulation
[Webinar Recording] Your DBS Questions Answered
When DBS Powers Down: A Personal Account
more about the speaker
Dr. Joohi Jimenez-Shahed is the Medical Director of Movement Disorders Neuromodulation & Brain Circuit Therapeutics at the Icahn School of Medicine at Mount Sinai. After completing her undergraduate degree at Washington University in St. Louis, Dr. Jimenez-Shahed received her medical degree from Baylor College of Medicine (BCM) and Neurology residency training at Duke University Medical Center. She then completed a fellowship in Movement Disorders at the Parkinson’s Disease Center and Movement Disorders Center at BCM. Her research interests lie in investigating the intraoperative neurophysiology of patients undergoing deep brain stimulation (DBS) for movement disorders and the application of wearables and digital health technologies to the care of patients with Parkinson’s disease.
THANK YOU TO OUR GOLD-LEVEL SPONSORS*
Live Well Today Webinar Series Presenting Partners*
 *While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.
*While the generous support of our sponsors makes our educational programs available, their donations do not influence Davis Phinney Foundation content, perspective, or speaker selection.
Thanks for Listening!
To share your thoughts:
- Leave a note in the comment section below.
- Ask a question by emailing us here.
- Share this show on Facebook.
To help out the show:
- Leave an honest review on iTunes. Your ratings and reviews really help, and we read each one.
- Subscribe on iTunes.
Listen & Subscribe
Apple Podcasts | Stitcher
*The Third Season of the Parkinson’s Podcast is made possible through generous support in honor of Dr. Margaret Hilgartner.