Receiving a Parkinson’s diagnosis when you’re young is overwhelming enough. Being a woman with a Parkinson’s diagnosis adds an additional layer of complexities and challenges. In this panel discussion, our YOPD Women’s Council talked about the added challenges women living with Parkinson’s face as it relates to contraception and pregnancy.
You can watch the video below.
To download the audio, click here.
You can read the transcript below. To download the transcript, click here.
Note: This is not a perfect transcript, but it’s close.
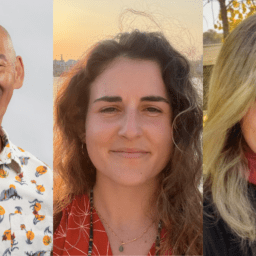
Melani Dizon (Director of Education and Research, Davis Phinney Foundation):
If you like the transcript, you can just keep it going on your screen if you don’t like it then you just click the little arrow, and it’ll say hide subtitles, so you don’t have to, to get it.
Okay so Karen, can you just tell us who you are and how you came to be part of the Women’s Council?
Karen Frank (Davis Phinney Foundation Ambassador, YOPD Women’s Council Leader):
Sure. Hi, my name is Karen Frank. I was diagnosed with Parkinson’s disease at age 47 three years ago. I have practiced professionally as a nurse anesthetist for over 20 years and when I was diagnosed with Parkinson’s disease, I retired from that profession.
Now I spend my time as an ambassador for the Davis Phinney Foundation, I do a lot of volunteer work with physicians and nurses who need help with overcoming drug and alcohol addiction, and I run a coaching business to help people with living well, mainly recovering from addiction, but I’d like to get involved and living well with Parkinson’s disease so, that’s kind of my background, and I’m happy to be here today.
Melani Dizon:
Great, thanks. Soania.
Soania Mathur, MD (Davis Phinney Foundation Board Member, YOPD Women’s Council Leader):
Hi, I’m Soania Mathur, I’m a family physician and a patient, having been diagnosed over 22 years ago, I believe.
I’m a proud member of the board of directors for the Davis Phinney Foundation and I work with a number of other organizations. I also have a website called Unshakeable MD, where I do talk about living well with Parkinson’s disease, and that sort of thing and I also am a co-founder of the PD Avengers, which is a global advocate group. I’m happy to be here.
Melani Dizon: Thanks. Kat?
Kat Hill (Davis Phinney Foundation Ambassador, YOPD Women’s Council Leader, YOPD Council Leader):
Hi everybody, I’m Kat Hill, and I was diagnosed with Parkinson’s disease at the age of 48, and at the time I was the director of midwifery for a large inner city midwife practice. I’ve delivered over 800 babies, and I am also the proud mother of three children.
And I have a special interest in pregnancy and contraception, everybody in my office was either in need of one or the other types of health, they were either pregnant or needed to not be pregnant, so this is my clinical area of expertise.
And since I retired, I’ve been doing advocacy work. I’m a proud member of the PD Avengers that Soania founded. I helped found, co-founded The Women’s Parkinson’s project, I’m an Ambassador for the Davis Phinney Foundation.
I am going to be having a book published soon by Haverly Press called “Being Well.” And I really believe in living well every day, even on the hard symptomatic days, so you’re going to see me with sort of a tough symptomatic day folks, but I’m excited to talk about this and hopefully Heather Kennedy will be able to log on here, she’s trying to get the link so there may be a few other people joining us throughout.
Anybody else know you want to introduce yourself? Anybody else want to jump in here or should we dive into the content?
Melani Dizon:
Yeah, just go for it. I will manage the chat and the emails about links and everything.
Kat Hill:
Sounds good. Alright, so first off glad you can join us today and I think this is an area that we don’t know a lot about, and I just want to say having said my credentials here, I really think that Soania is going to be the expert in this area because I think Soania is the only one among us, that has been pregnant while having Parkinson’s and having dealt with it, so poor thing, she’s like, what, I’m on five minutes and I’m on the hot seat. So even though clinically I know a lot about this area I don’t, I didn’t treat anybody ever in my practice that had Parkinson’s and has had a baby. But I think there’s lots of questions that come up in managing chronic illness, when you’re pregnant.
So, I’m going to talk about it sort of globally. And then but what I really want to say is, we are not experts there’s not a lot of data about this so we are in no way making medical recommendations about what you should or should not do.
We’re here more to have a discussion about perhaps what areas we need more research about, and maybe the little bits of things that we’ve learned or each of us have maybe experienced but again this is not to, in any way, is not meant to negate the need for you to talk with your provider if you’re thinking about a pregnancy, want to have a baby, or want to manage your contraceptive or hormonal needs differently.
Okay, so it’s kind of unchartered territory. I’m really happy to report though that this topic is gaining a lot of traction internationally. We are starting to have more dialogue around what it’s like to be female and to have Parkinson’s disease.
Excuse me, and that includes things like pregnancy, perimenopause, post menopause, hormonal replacement, contraception and that’s in some ways more unique to the female experience.
So, we’re just going to be part of the dialogue. What I’d like to say is as a clinician who’s had the privilege of working with many many pregnant women that that women’s needs don’t suddenly change just because they’re pregnant, some diseases we know may have less or fewer symptoms during pregnancy, some diseases may experience more symptoms during pregnancy.
It’s complicated when you’re taking medications to treat symptoms when you’re pregnant. And because we can’t ethically study medicines and pregnant women. We can’t say, okay you 25 pregnant women who have Parkinson’s, we want you to take all of your medicine. And then you 25 women over here we don’t want you to take your medicine and then let’s see how your kids turn out. Right? That’s not ethical. Right?
But we can do that in rats, and we can do that in other in other mammals, but for that reason medicines are often categorized in a letter system, A-X, so it’s A, B, C, D and X. A medicines are medicines that we know are absolutely safe, we’ve tested them, we know pregnant women have taken them forever, and we know they’re safe. There are very few A medicines. Even things like acetaminophen and prenatal vitamins aren’t all labeled A.
So those are more the B medicines, we know that women have taken them, they haven’t had poor outcomes. We feel safe prescribing those. So, A and B are somewhat the same. X are those things that we know are absolutely not safe to take during pregnancy.
The reality is most medicines fall into that C category, which is, we need to weigh the benefit to mom and try to minimize any harm or side effects to the growing fetus, to the growing baby.
And as an advocate for women, and for mothers, it’s a really fine line and a dance that needs to be done and I think it’s important that we look at individuals because if we tell women that they can’t take any of their medicine during their pregnancy, they may not have a quality of life that’s going to work to manage a pregnancy. We also know the first trimester of pregnancy is the most sensitive time as the baby’s developing and so maybe we can work to modify medicines that first trimester and work to modify symptoms later. So, those are kind of some general guidelines. In terms of contraception, I’m just going to give a little bit of information and then I really want to open it up to discussion if that feels okay. We seem to find that more women are diagnosed with Parkinson’s around menopause and that’s pretty well documented, we feel pretty certain that. Now some of that reason is age because one of the risk factors for getting Parkinson’s is just getting older.
And we know currently that, at least in the United States we have more men that have Parkinson’s than women, so another risk factor could be being male. We’re going to kind of skip over that part today.
But for women we wonder if perhaps declining hormones, maybe estrogen, may affect their ability to get Parkinson’s. So that’s a question mark that we don’t know so, we hypothesize around that, we think about that and we’d like to see more research done in that area. And if that’s the case, if we find that to be the case then is supplementing our estrogen a helpful thing or a protective thing and that could be protective not just for women but potentially for men as well.
If estrogen could be protective, it’s not just women that could protect themselves with estrogen, there are other treatments that use other hormone treatments for male cancers for example and so I think it’s an untapped area of research.
So that’s sort of what we know, or rather, an awful lot about what we don’t know. And what I would advocate for all of you that are out there saying well gosh this is really not very informative; they’re telling us all the things they don’t know what I really would love for you to do is have a dialogue with your provider, if you’re noticing your symptoms are different. And you are having your periods, we know that women seem to have more symptoms the week before their periods, which also would indicate that as that estrogen level is dropping, or as my friends in the UK say, the “ee”-strogen level, the “ee”-strogen is dropping, that they have more symptoms. Talk to your provider about it perhaps there can be some things that can be done to keep you less symptomatic that week before your period.
If you’re thinking about getting pregnant, talk to your providers about it. Be proactive about it don’t automatically think well I absolutely can’t have children. If that’s something you’ve always wanted, theres ways to do that. So, so don’t give up and have hope, even though we don’t have data, talk about it.
All right, I’m gonna I’m going to jump off my little soapbox here and I don’t know if that was helpful, but, and I’d love to just open it up for discussion, so I’d love Soania, if you’re open to sharing a little bit about your experience about pregnancy and Parkinson’s. I’d love to hand the hand the mic to you.
Soania Mathur:
Sure, I can talk a little bit about my experience. It’s a while ago, my oldest is now 22 and I was pregnant with her actually when I found out about my diagnosis, which was an interesting time to receive that news versus trying to enjoy you know your first pregnancy and all the joys and anticipation of the coming of your new you daughter. I had two more daughters after that.
So, my daughters are now 22, 20 and 16. So we’re talking about a little while ago.
So, when I was first pregnant, it was an interesting time, and that people really didn’t know what to do with me. So, when I went back to my OBGYN and said, I have Parkinson’s disease, then he was kind of like, oh, okay, well, what do you do now.
So, it ended up being just he just followed me along as anyone normally would. The second time when I became pregnant, I went to genetic counseling and then I saw, you know, a high- risk OB specialist and again I don’t think they knew to do with me but everyone and their partner was in the room when I was delivering, it was just a packed room, because they didn’t know what to expect. So really my experience was, and this 16-year-old when she was born, it was pretty much like the first time, so the experiences were so varied and that’s truly because as you said cat, we don’t know enough about how to deal with women in during their pregnancy and Parkinson’s. There are far more questions than answers sometimes so, we have to kind of go by experience as you said.
As far as I know from the reading I’ve done, there’s no increased risk for fetal abnormalities or congenital defect in women that have Parkinson’s disease, which is obviously a promising thing, but the management of symptoms is sometimes difficult, also as you said.
For the first two pregnancies I wasn’t too bad because there really wasn’t a lot of medications, it was still early in the course my disease. By the time I got to my third pregnancy, I really needed some help, because the experience of pregnancy, as you know, has its own stresses on your body and you add Parkinson’s into the mix and you’re kind of stuck so at that time as we still believe now, the safest medication that we have for Parkinson’s disease that would be, you know, not the Class A or even necessarily Class B but is levodopa/carbidopa.
And so, I ended up taking a little bit of that, I wait until after the first trimester, because again, very unanswered questions, so I kind of suffered through my first trimester and then start taking it I believe in my second.
So, yeah, that was my experience, very, very uninformative considering there really wasn’t many answers then, as I’m sure people find it difficult to find answers now.
Kat Hill:
Soania was it scary for you? Did it feel like uncharted territory to be getting sort of, to not really know, but to be symptomatic enough that you needed medicine? You know, I wonder if that was frightening for you.
Soania Mathur:
Well, it wasn’t as much frightening as confusing, I think. I mean, as I said, I didn’t take anything for any of my first trimesters in pregnancy, because I felt, you know, I knew that was sort of the most formative time. For the first two, I didn’t take anything at all I just kind of suffered through it, but my symptoms were mild enough that I could do that. By the third time, as I mentioned, I had to go through. So it wasn’t, it was not, I mean I can imagine it would be frightening. I think a little bit with my medical background I felt a little bit more confident about knowing what I knew and not knowing what I didn’t know.
So, yeah, but it can be very, you know you expect to go to your physician and be told, this is what you should do. And as we’ve seen with women in Parkinson’s in general, that’s not necessarily going to be the case.
Kat Hill:
Yeah, and symptom wise, did you find that that it changed? Did you feel different pregnant than you did non-pregnant in terms of your symptoms?
Soania Mathur:
Definitely, I mean, definitely the symptoms were there when I was on medication, but also, I felt that my symptoms were accelerated a little bit during the pregnancies, they seem to come back, pretty much up back up to baseline, but they may have been a little bit worse during the time that I was pregnant but as I said as hormones start to come back to normal it was a little better than it was during pregnancy.
Kat Hill:
Thank you. Thank you for sharing so candidly.
Heather Kennedy (YOPD Council Women’s Council Leader, YOPD Council Leader):
Did you say that hormones go back to normal at a certain point because I’m still waiting.
Soania Mathur:
Oh, me too now Heather.
Heather Kennedy:
Because now we’re into menopause, which is really fun.
Kat Hill:
I say I’m 24 years post-partum. My youngest is 24…So does anybody else have anything to add sort of to the pregnancy discussion? As a midwife, I would think also that, like I think about I did water births and I did a lot of labor support, that I’d want to be careful with straining muscles and positioning and those kinds of things during labor, because we all know that we have more trouble with muscle tension and muscle related issues but mechanically, from a mechanical standpoint, I think that there’s no reason to think why mechanically a baby can’t be born just fine to women with Parkinson’s disease. So, pillows and extra hands and contraptions on beds can do wonderful things to help women be comfortable, whether they have Parkinson’s or not. Comfortable as comfortable gets in labor.
But that I think that there’s lots of creative ways and there’s great pain management for labor as well, so, that could help us.
Heather Kennedy:
May I mention a very useful item for people that have trouble rolling out of bed with Parkinson’s, especially when they’re pregnant?
Kat Hill: Please.
Heather Kennedy:
I came across this quite by accident after Kat left. Kat was a huge help to me post-surgery. And as you know with brain surgery you can’t really lift or put your head below your heart and all that, but there’s this pulley system that you can buy, it links on to the bed, and if you have like a headboard it’s even easier but if you don’t you can you can fix it between the mattresses, it clips on, you can pull yourself up with these loops and it helps so much I would imagine for pregnancy it’d be really great.
I can’t even imagine being pregnant and dealing with Parkinson’s. I mean, what women are carrying with that is just incredible and awe inspiring, I’m listening. I can’t even imagine. I’ll put the link here.
Melani Dizon:
What would you say about morning sickness for during pregnancy and does that impact medication absorption and what are some things that people, you know can do if they have really bad morning sickness?
Kat Hill:
Sure. So, not everybody, it’s interesting because morning sickness always gets the really dramatic bill, right? You know, on any of the films, you think, oh she’s vomiting in the morning, that’s a sign that the woman is pregnant. So, nausea and fatigue are really much much more common in pregnancy, especially in the first trimester, than is actually vomiting. But if somebody’s feeling yucky and having trouble with nausea and vomiting you produce a lot more stomach acid when you’re pregnant. So, I would give a woman with Parkinson’s the same advice that I would a woman without Parkinson’s, is to try to keep that stomach acid diluted.
So, nibbling on things kind of around the clock and for Parkinson’s folks on non-protein, snacks, so that they can tolerate their medicines alright. But if somebody is having sort of intractable vomiting, that’s a problem regardless of whether they have Parkinson’s disease. So keeping that stomach acid diluted, being careful about when you time your protein intake, I would recommend a high fat, high protein snack at night, and often women that are pregnant are getting up to go to the bathroom in the middle of the night and so I often recommend keeping a little bit of a snack by the toilet in a Ziploc container so that they can nibble a little bit, and have some fluids and some carbohydrates when they get up in the middle of the night, so they don’t wake up on that totally high acid stomach.
So that would be my take on that, and I think also recognizing that metabolisms of medicines might be a little bit different, and also something that I’d recommend is if you’re thinking about a pregnancy again, bring it up and talk about it early and talk about how you might manage your Parkinson’s if you’re planning a pregnancy. Only 50% of pregnancies in this country are planned.
So, if you find yourself pregnant and have Parkinson’s, and I would recommend going in right away and talking about it and talking about kind of what the trajectory should look like or some of the things that you can be doing.
You can also do things like take your prenatal vitamins at night with dinner, if those are making you nauseous. So, there’s some strategies that you can work on so that you can tolerate medicines, but also trying to minimize sort of some of the complications that can happen with any pregnancy. So, did I answer that okay Mel?
Melani Dizon: Yes, absolutely.
Kat Hill:
Okay, Miss Karen.
Karen Frank:
Yeah, I was racking my brain for how I could offer some value here in this conversation because I’m perimenopausal, I’ve never had children, and I got diagnosed with Parkinson’s disease after I had my last period. So, I was thinking what can I do?
Kat Hill:
And you are female.
Karen Frank:
Yeah, I am female, but I was I was talking to Mel beforehand, and she said, well you’re medical and I started thinking about, you know, when I used to do anesthesia for OB.
There are some considerations that you might want to keep in mind with Parkinson’s disease and having an anesthetic, whether that’s an epidural or a spinal anesthetic or even an emergency general anesthesia, or even just from pain management, things like managing post- operative or inter operative nausea and vomiting, blood pressure, things that are affected by the physiology of pregnancy and also to keep in mind with Parkinson’s.
One of the things that came to mind for me is that some people take MAOB inhibitors, which are drugs likes Selegiline, Rasagiline, those drugs, a lot of people in medicine, aren’t that familiar with MAOB inhibitors, in terms of neurologic disease. They’re more familiar with what’s called an MAOA inhibitor which is given for psychiatric conditions as an anti-depressant, and those drugs famously have a lot of food interactions and drug to drug interactions and so people in their mind they hear that you’re on an MAO inhibitor and they might think of those things.
But one concern, if you are going to have anesthesia for labor and delivery, would be to come armed with some information for your anesthesia provider about what nausea drugs that you should not be getting. Drugs such as Metoclopramide or Reglan®, Haldol®, Haloperidol, sometimes given in low doses for nausea. Those are not very good in the setting of Parkinson’s disease because they work on dopamine receptors, they are much safer drugs.
So, I know the American Parkinson’s Disease Association has a little card, and it has drugs which perhaps to be given with caution in people with Parkinson’s disease so that’s helpful.
And I do believe that the Parkinson’s Foundation has a kit called “Aware and care,” and that is a kit, which is supposed to be geared toward the peri-hospital experience, and if you are going to be having a baby, that might be helpful information. It has sort of sample letter that you can provide about your condition and medications that you take and various other things. But, you know, one other thing is that people with Parkinson’s sometimes have fluctuations in their blood pressure.
They have sort of an autonomic dysfunction. And, you know, it’s very well managed in the setting of anesthesia with medications and fluids but it’s something to be aware of and probably discuss with your anesthesia provider if you get lightheaded when you’re standing up. If you have low blood pressure as a baseline with your Parkinson’s disease, that would be helpful to let someone know.
Kat Hill:
Karen would it be helpful, I often had patients who had medical challenges during pregnancy, they would schedule a consult before delivery with the anesthesia team, so that it was all documented in their record kind of about what the plan, should be, could be… Again, I’m asking women to take a lot of ownership, with this part and advocate for themselves before labor. Labor is a hard time, you know when you’re in the midst of having a baby in the hospital, it’s a hard time to be making decisions in the moment. So, planning ahead is a really good plan.
So, planning ahead, is a really good plan. I’d like to also mention that the American Parkinson’s Association has good things but, the Davis Phinney Foundation has some great tools about getting ready for a hospital stay also on their website and in the Every Victory Counts Manual so there’s lots of tools for women to be proactive with their stay and this is across the board, I’d like to say, I know Heather and I had some of these conversations about, you know, going into any surgery, so this is not just unique to being female, it’s unique to being human.
Karen Frank:
I’m seeing Heather’s comment here about taking medications when you’re in the hospital. I do think it’s important to bring your medications with you. First of all, some of the medications aren’t available on formulary at every hospital. I take extra carbidopa and that’s very important.
Heather Kennedy:
They wouldn’t let me access them.
Karen Frank:
That is a problem, that is a problem.
Heather Kennedy:
It was unbelievable, unbelievable. I was dystonic and twisted and they wouldn’t let me get my own meds.
Karen Frank:
That’s one’s difficult. I know when I was in the hospital, I had a similar experience, but the pharmacist actually took the medications, they examined them, they looked them up on the computer and made sure they were what I said they were, but some of my medications came from Canada, they aren’t even available in the United States, such as Domperidone. So, you know, they really had a field day with that one, but I kind of, you know, had them in my bag anyways, and had that in my corner, but as far as the pre anesthesia workup you were saying that a lot of people can go in ahead of time, Kat and talk to an anesthesia provider.
That’s pretty routine for many types of surgeries and it’s called a pre anesthetic CPAP which stands for… I don’t know even what it stands for that horrible. I just say CPAP. But you know where patients are seen, and they can pre look at their labs and their meds and make recommendations.
Kat Hill:
CPAP stands for continuous positive airway pressure.
Karen Frank:
That’s a different CPAP.
Kat Hill:
I was like okay, good, I know something, me me!
Melani Dizon:
That made me think about doing the consult, you know, a lot of times you will have a primary OBGYN, right, that you’re planning on going through the whole process with, they know about your Parkinson’s, they’re all tuned in, everything’s going to be great, and then they’re off. Yeah, right? So, having those conversations with the whole team is, is it.
Kat Hill:
One thing that’s nice about having an electronic medical record which is now pretty much the standard of care everywhere, is that those notes, and those directives should be noted in your medical record. And I think being proactive about that is really important. I practiced in a group practice setting, and we had to keep thorough notes, there were 13 of us. So, seven core midwives but any of my partners could be on call during the time of delivery, so it was important that we take really copious notes and keep an up to date, what we call problem list, which is not my favorite term, but a lot of notes were kept specifically in that area to communicate between providers, so I think that’s an excellent point Mel, and that also goes for, you know, just being proactive, asking for those appointments.
Some hospital systems, and I know not everybody delivers in a hospital system, but when you have a chronic illness, I think it’s a good idea to deliver in a hospital system. So that you can have the tools available that you need and being proactive about that is important. And what I learned a lot from Heather’s case, is that even if, in a center for excellence, in a highly rated facility that does a lot of work with people with Parkinson’s, they don’t always have everything ready for you at the hospital.
So, I think, asking the questions, being really direct and saying hey I heard a webinar, and I’m having a procedure done, I need to have my gallbladder removed, oh gosh, I remember they said to talk about it ahead of time. So as soon as you know that you’re having a procedure done, bring it up. I’ve got Parkinson’s disease. Get your medicines together, get somebody to help advocate for you if you’re not able to advocate for yourself.
Soania Mathur:
Yeah, I think that’s really important Kat, that you mentioned that last part because I think that when you’re in a situation, especially say pregnancy and your about to, you know, you’re going into labor, you’re not necessarily going to have the fortitude to be able to advocate for yourself very well so having things written down and having a, hopefully a care partner or someone go with you that can advocate for you on your behalf. I think is really important.
The one thing just to get back to the medication piece is that amantadine we know is not good for pregnancies and for the growing fetus, so that’s one thing that you know if you happen to be taking and you find yourself pregnant you need to, you know, discuss that with your physician right away or, you know, try and discontinue your use of that before you get to them.
The other one thing to remember if you bring your own medications is that certain things are not necessarily the best for breastfeeding if you go that route either, so you need to check with your physician about that. I mean things like dopamine agonists, for instance will suppress prolactin which will interfere with your lactation in the postpartum period, so medications are one thing that we know some things but not everything so it’s important to discuss the possible scenarios with your physician before you get into that situation.
Kat Hill:
And many health systems where you deliver, sorry, and then Heather’s up, when you deliver, often you’ll have the opportunity to meet with a lactation specialist in the hospital. I think that that’s imperative to do that before you’re discharged or make arrangements to do that and there’s lots of resources available, but I agree with you, having things written down it’s really helpful and having somebody who can help advocate for you if you’re not in a headspace to do that and that’s again universal. Heather, all yours.
Heather Kennedy:
I was just going to mention that in this tech innovation seminar that I’ve been attending, with Rui and John Dean, and a bunch of others, they’re talking about having some sort of a band that we could wear that could be scanned, but there are so many privacy issues in particular in America. Because oftentimes someone will be traveling or something unexpected will happen like a fall or, you know, an accident.
And so, we don’t have time to prepare so to prepare ahead, at least fill out that little form that you get from the Parkinson’s Foundation that Karen mentioned, I think it was. You talked about the kit you can order, “Aware and care” kit. That is so important to have that with you, just taking your wallet and having your phone, not only your ICE contact but under that, just for the emergency personnel because that’s what they’re going to be looking for, I-C-E, in America anyway, and make sure that you list your medications there, just have them somewhere in case you can’t talk or in case you can’t communicate or in case your loved one is not with you because you just never know it’s better to be prepared. So, whether you’re pregnant or not or whether you’re, you know, whatever’s happening your life we have a body that we have to contend with.
And we have more to our body than just Parkinson’s. So, let’s be prepared ahead of time. I wish I had thought of that before my kidney surgery and my shoulder surgery and some other things that were more immediate.
Kat Hill:
I take a photograph of my current prescriptions, and I fold it up, and I stick it in my wallet and all that does, is it just, because I often will just have loose pills or in my pill case, right, I mean who wants to carry around the big, huge, you know bottles, but I have a photograph of that in my wallet. And I think that that’s helpful for those same reasons Heather, for the same reasons. So yeah, Karen, you.
Karen Frank:
I also received an Apple Watch for Christmas, which was great I never had one, and on the Apple Watch, it has, oh it’s talking to me, it’s actually listening. It has a sort of a medical ID, that’s digital, and you can actually program all your medications any allergies that you have, any pertinent medical information or conditions, contact people, your doctor’s name and number.
It’s actually pretty cool feature of the Apple Watch so if anybody uses an apple watch that might be helpful. That was one thing and then Kat, I also wanted to mention something related to pregnancy and lactation.
A friend of mine who doesn’t have Parkinson’s was taking down Domperidone to help with breast milk production. Do you know anything about that? I know that’s a common medication for people with Parkinson’s.
Kat Hill:
I do actually and prescribed it often to women that were having lactation issues in terms of milk supply issues. So, I know that it’s more complicated to get now on many, it’s not carried in the formulary, so it’s something that we had to be sure was stocked postpartum. I also do want to say that you know it’s been five years since I’ve been practicing in the hospital so while I try to keep somewhat up to date about what’s going on again, I’m going to give my disclaimer that I’m not the most up to date on all those pieces but yes, it can help with lactation for sure. And I also want to add I think you made a really good point Soania that some of the medicines for Parkinson’s can be detrimental we know in the first trimester.
But definitely talk to your doctor because stopping some cold turkey can also be really harmful for you so, so just being aware of all of it. That’s why if you can plan your pregnancy, plan ahead, talk about what’s good, sometimes we can shift a medicine that is see are known to be safer like carbidopa/levodopa, try to futz with those a little bit to make it safer
Soania Mathur:
Oh absolutely. Especially I mean when you’re talking about some of the MAOB inhibitors for instance and other medications that can be very dangerous to stop the cold turkey on your own. But amantadine is really ones that you should discuss with your physician about because if you’re planning to become pregnant that’s one that you probably want to change.
Kat Hill:
I also, I’d like to shift a little bit I think we did a really good job does everyone feel good about kind of what we covered about what we know and don’t know about pregnancy?
Because I do want to spend some time talking a little bit about contraception, too. And, and I wouldn’t be a good midwife if I didn’t talk about both in the same breath. So, if you don’t want to get pregnant, I think it’s also important that you take steps not to become pregnant if you’re sexually active and think about, and talk to your provider about what’s a way not to do that and there’s lots of contraceptive options out there that are absolutely compatible with Parkinson’s, and Parkinson’s medicines, so I would advocate that an unwanted pregnancy can be a stressful thing, and can be physiologically challenging on a body so I would really encourage you to not think that that’s going to complicate things, trying to get on a contraception.
There are even some non-hormonal, there’s lots of non-hormonal non medicine contraceptive options. And I wouldn’t be doing a service unless I talked about both.
I know that I used a copper T-IUD that didn’t have any hormones in it for a long time and I IUDs are the most common form of birth control in Europe. In the United States we haven’t quite caught up with them in terms of being a favorite but it’s nice because it’s implanted in an office visit and then you don’t have to think about it for several years and most women report really high satisfaction rates with that as a contraceptive option.
There’s the Mirena® IUD also that has small amounts of progesterone that mostly stay localized to the uterus, and some people will have more systemic effects because anything that’s in our body you can’t say oh it just stays right there, right, there’s little bits of it that seep into the bloodstream, but that can be a useful tool and some women really love that they have lighter periods or no periods at all. Now that doesn’t necessarily mean that they’re not having fluctuations cyclically with some of their estrogen levels so I’m not sure that we can say that it would prevent dropping estrogen levels, and some of that what would be before your cycle time may be increase in symptoms, but it may help theoretically to have that little bit of progesterone on board. So that may be an option for women who really know that are not interested in being pregnant who are sexually active and are pre-menopausal, right, we’re getting narrower and narrower, so I’m talking to like six of you out there but, no, I’m kidding.
That could be a really helpful tool, so just remember that those tools exist, and yeah, that’s my soapbox for that one. Does anybody have anything else to add to that? Mel, are you get many questions coming in?
Melani Dizon:
I was just gonna say if anybody would like to share some questions in the chat, we’ve got these four women who have so much insight to share. Maybe just a question your curious about for women in general women’s health in general, or because you’re thinking about becoming pregnant or you are pregnant. Any questions are totally open.
Kat Hill:
I thought I might also add, I was part of a kind of an informal research study that was asking women, were providers that they’re seeing asking about their periods or about their cycles or about menopause and what we’re finding is that most providers are pretty, other than those of us doing OB and reproductive health are pretty uncomfortable bringing it up in the exam room, so I think it’s really important that we as women, recognize that menstruating and going through menopause is a really integral part of our experience.
If any of you out there are having hot flashes, or are currently pregnant really know how really integral, it is, that it’s important to have the discussion because we, our providers may be uncomfortable bringing it up, they haven’t been trained in these specific areas, so we need to be comfortable bringing it up, hey, I’m really having these hot flashes. I’m noticing I’m more symptomatic when I’m having the hot flashes, you know, is there something we can do? And, yeah, Karen.
Karen Frank:
Yeah, I actually just went to my GYN for a hormone check because I mentioned that I was peri menopausal and I started on hormone replacement therapy, about six months ago.
And, you know, between being a newlywed and being perimenopausal and trying new medications I mean I have anxiety and depression as non-motor symptoms of Parkinson’s and my neurologist along with my psychiatrist recommended that I switched to a new anti- depressant that have more coverage for anxiety associated with Parkinson’s which was an SNRI, which was desvenlafaxine, I think it’s a generic name, but that has some sexual side effects and it can blunt pleasure during sex, if you will, like you, you just can’t climax I mean you could go like an hour and think you’re going to and then you just can’t, and I mean you know it’s difficult to talk about, but sex is important, that’s part of life it’s part of being happy person, you know, it’s happiness for my husband as well, so you know it was nice to be able to talk about that and I wanted to bring up one thing, this is not medical advice by any means, and I know people have different opinions on medical cannabis, and that kind of thing, but that actually is something that can really help with libido, and sexual pleasure and people that are having side effects from the medication, and my neurologist said that.
He also mentioned that you can skip your dose that afternoon, of your SSRI or SNRI and then take it after sexual intercourse, or sexual activity Later in the night. So, I thought those were interesting suggestions that people might want to look into or investigate.
Kat Hill:
And Karen, that’s a really really good example of you bringing it up to your provider. Our providers also can’t read our minds and while I believe that it would be good practice for us to encourage providers to ask more questions around women’s health, they can’t automatically know that we’re having trouble. They also, not everybody experiences every possible side effect of medication. So, if we don’t bring it up and advocate for ourselves, like saying I’m too flat, I don’t love that, I love that my anxiety’s gone but I don’t like that I can’t have an orgasm, and I’m newly married you know that that’s affecting my quality of life. And so is there a way that we can work with it and that’s a beautiful example of coming up with an individualized plan for you to try some trial and error. So yeah, Heather.
Heather Kennedy:
I am so grateful that you brought this up Karen because it’s kind of like have you ever had a massage. And you realize, wow, I was really tense, or you take a yoga class you think I’m going to do this every day it felt so good and then you don’t but that’s another story.
But you realize how tense you are, so when you don’t have quality of life when you’re experiencing such consistent chronic pain. I believe what happens is that we become, that becomes normalized.
We cannot let the absence of pleasure and joy, and even orgasms become normalized because life needs this, we would be missing the joie de vivre, we will be missing that essence, we will be feeling less alive and what is worse for a neurologic patient, than
feeling diminished even further than going smaller with your voice and being caved in on your body and not being able to move much and then also lacking that pleasure, we need it.
It is our God given right it is something that everyone should experience, you know, it’s just a human right, I believe it. So, I cannot stress enough how important that is what Karen just said and thank you for being brave enough to bring that up. We’ve all tried those different inhibitors and they do flatline you, they make you feel like “wonh, wonh,” it’s like, well I’m not upset, but I’m also not feeling anything.
Kat Hill:
And I want to say that I think it was super brave of you Karen and I love that you’re a newlywed but I’m also going to say after my husband I’ve been married 31 years. That’s a long time. I’m really only, you know, 26 but even that’s important to us, you know, our health as a couple is complex and layered, but a part of that is certainly the intimate part and I’m currently and you know as a woman in my 50s really trying to maximize and store and collect and challenge myself to find joy in every moment and every day, maybe not every moment but every day at least, and the more the more joy we can collect, the better off we’ll be so I don’t know.
Heather Kennedy:
You do walk that talk I’ve seen it. You actually, I’ve seen you catch yourself saying something, and you’ll switch and flip it and use different language, even to sort of promote the idea that you have some control over your situation.
Kat Hill:
I pay Heather every month a small stipend to come on and…
Heather Kennedy:
This is so universal though, this goes so far beyond Parkinson’s, right? Like we can all relate to this as women and as just as human beings, so I really appreciate you guys bringing this all this up but one more thing that I thought of too. Staying connected to other women is so important, especially when we’re going through these transitions because that’s where we get the wealth of our information from. So, I’m even taking notes as I tend this myself so thanks.
Kat Hill:
Soania, do you have any tidbits about how you find joy in your day? We’ve been kind of dominating this. Any advice to somebody maybe that’s diagnosed, that’s in their 30s and contemplating having a baby? Do you have any words of wisdom or advice? I always look to you as somebody who has walked this path longer than I, so I’m so appreciative of your insights.
Soania Mathur:
Well, I may have been on this path, but I really was on a good path for the entire time. It took me a while to figure out the fact that I wasn’t gonna wake up one day and this will all be done, you know that you know wake up all flexible and supple and you know, life would be back to normal.
So, I did avoid it and kind of, you know, buried myself in busyness of life for a long time before I came to the realization that this wasn’t going to change. And I didn’t have control over that diagnosis, but all I had control over was has been to face the challenges that I’ve been brought, and that I was becoming a pessimistic person and that’s not who I wanted to be. And then optimism for me to become a choice. Not an easy choice, but a choice, nevertheless. Because there is that moment in time between a stimulus and a reaction that you have in order to make a decision about how you’re going to react to the situation.
And that’s sort of become my mantra that you know optimism is a choice and I choose to be optimistic and hopeful and helpful, because the fact is, what’s the other choice? It’s not a great option.
So, and that’s the way I looked at, you know, when it came to my daughters, yes, I didn’t know I had Parkinson’s disease at the time I got pregnant with my first child, obviously, but I didn’t let that slow me down, you know, I wanted to have more children. I wanted to have, you know, at least two or three kids. And that’s what I ended up doing and I will say that they have been probably the stabilizer in my life, you know they brought me joy and they, I worried at first, I will say that.
I mean I went through a period of time, especially after my first child was born that I would look at her and think, you know, am I going to be a burden in her life? Am I actually going to be able to see her during her first milestones? Am I going to be an active mother? Am I going to be able to keep up with the other mothers? And those are very natural and normal fears I think that every woman has, regardless of whether they have PD, but it’s obviously amplified for women that have a chronic illness. But I will say that you know you learn to adapt, you learn to modify the activity, according to your capabilities, you learn to ask for help.
you also will see that, you know, for me, I know that this experience has brought my daughters, a sense of reality that life isn’t always going to be perfect, but how they face the challenges will determine what kind of people they are.
And they’ve learned empathy, they’ve learned, you know, charity, they’ve learned a lot from this experience so those fears are normal and natural for any woman that is in that situation, but I will say that, you know, it’ll be the greatest blessing that you have, and your children can learn from every experience, including this one.
Kat Hill:
Yeah, I really love how we, we started out to talk about these specific things that we don’t know a lot about and all of our conversations come back to the core kind of the essence of being human right. We all have choices, there’s very few humans that I know that haven’t had adversity somewhere in their lives right and how we react to it really will define who we are.
And I think when it comes to being female to being wives and sisters and daughters and mothers and cousins and you know all of the things, we carry with us often that caretaker mode, and it can be a gift to our fellow women, including our daughters, and our sons, about how we how we interact and how we grow through the challenges that we have. So, I think it’s, um, I love that we come back to the big philosophy of being human, even though we’re talking about these really specific subjects and I and hope our listeners our viewers feel like they were able to glean, a little bit of insight.
I know we said a lot about what we don’t know but I think as a community we can really grow if we can keep having the discussions and keep talking about it, and being honest and open and Karen I want to thank you again for your bravery, same with
Soania I’m always picking on you about, you know, you’re my go to partner in a lot of these things but I really appreciate you being candid about what it was like to be pregnant and Heather, of course you inspire me every day so.
And I want to also thank Mel and the Davis Phinney Foundation for giving us the place to come and talk about some of these things because I think it’s really powerful. And I think that women can change the world and maybe we’re starting to do that a little bit here with our conversations. So, Mel, is there anything else you want us to touch on?
Melani Dizon:
No, I think you guys nailed it. I really appreciate you guys talking… Heather, yeah.
Heather Kennedy:
I just wanted to add there are some policymakers in play, not just in the United States but internationally, they’re trying to add the component of women’s health back into the system as it was removed when people were going toe to toe about abortion or no abortion and all that and that’s not what I wanted to talk about, but I just want to say there’s some policy changes that will benefit all, especially women in the reproductive years.
Kat Hill:
So, vote, too. Share your voice, share your stories, talk to your providers and vote. That’s all.
Melani Dizon:
Thank you everybody, thanks to all of you for joining us today as well. And if you have questions about this topic, feel free to let us know at blog@dpf.org. We are really grateful to have this community and these really amazing women to talk about these issues that are really front and center for a lot of people so thanks for joining us.
Show Notes
- There are still many unknowns about the effects of Parkinson’s medication on the health and safety of a growing fetus. Therefore, if you are pregnant, the number one priority is to consult with your doctor. They will help you to determine a plan for your pregnancy that works best for you
- The first trimester of pregnancy is the most formative time for your baby, so, you may consider lessening or eliminating medications during this time and resuming them in later months. But, as always, consult your doctor before altering your medication regimen in any way, as an abrupt discontinuation of medications can be dangerous
- Morning sickness during pregnancy (which for many women includes fatigue and nausea) may interfere with the proper absorption of your Parkinson’s medications. To help counteract this, consistently eat small non-protein snacks throughout the day to dilute stomach acid and alleviate nausea. Overnight, stomach acid can build back up, so consider keeping a small snack by your bedside to eat in case you’re up in the middle of the night
- If you are living with YOPD and are pregnant or are wanting to become pregnant, don’t fret! Simply be proactive with your care and explore and address any complexities that may arise. As soon as possible, make an appointment with your doctor to discuss a pregnancy plan, set up a consultation with your anesthesia team and surgical care team to discuss medications to avoid, and speak to a lactation specialist to ensure proper care for your baby, post-delivery
- You may consider packing a “hospital bag,” containing a few days’ worth of medications, a list of your active medications, a Parkinson’s fact sheet, as well as a list of your active symptoms for your medical team. The more prepared you are, the better
- For women with YOPD who do not wish to become pregnant, there are many contraceptive options available, either hormonal or non-hormonal. Talk to your doctor to discuss how each of these might interact with your Parkinson’s and what the best fit is for you
additional resources
What to Know about Hospital Stays and Parkinson’s
Aware in Care: Parkinson’s Hospital Kit
[Webinar Recording] Women and Parkinson’s with Dr. Michelle Fullard
Want to hear more from the YOPD Women’s Council?
You can find all of our YOPD Women’s Council recordings here.