June is National Safety Month, and in this post, we’ll highlight five ways to be safer and minimize your risks in order to live well with Parkinson’s.
Falls, infections, and swallowing issues are among the most common causes of injury, hospitalization, and mortality for people with Parkinson’s. Each of the items listed below can impact one or more of these risks.
EXERCISE
It may be surprising to start a list of ways to be safe with Parkinson’s with something that has inherent risks, but exercise can help you live safely with Parkinson’s in several ways. Further reduce your risk of injury by exercising with a buddy or with a personal trainer or physical therapist.
The American Physical Therapy Association’s clinical practice guidelines for Parkinson’s recommend 10 types of exercise with high quality evidence that they improve quality of life for people with Parkinson’s. Some of these types of exercise directly improve your ability to live safely:
- Aerobic exercise may reduce symptom severity and capacity to use oxygen, which may help with orthostatic hypotension.
- Resistance training may reduce symptom severity by improving strength, including strength of muscles involved in urinary incontinence.
- Balance training may reduce postural impairments and help improve balance and gait outcomes to decrease fall risk.
- External cueing can reduce symptom severity and work against gait disturbances and decrease fall risk.
You’ve likely heard the phrase, “Nothing ventured, nothing gained.” This is certainly true of exercise, and accumulating evidence increasingly suggests that this investment is worth the risk.
ACCESS COMPLEMENTARY CARE EARLY
Complementary therapies are used alongside traditional medical treatments. This differs from “alternative” therapies, which are used in place of traditional treatment.
Complementary therapies include treatment from a speech language pathologist, who can help with speech and swallowing, and occupational therapists, who can help you improve your ability manage your activities of daily living including eating, bathing, maintaining your house, and more. View our complementary therapies resource guide for more information about benefits of speech therapy, occupational therapy, and 17 other types of complementary care.
Many types of complementary care—including speech therapy, occupational therapy, and even physical therapy—help more the earlier you begin. For example, in addition to helping navigate changes in your speech, seeing a speech language pathologist before you regularly experience swallowing difficulties may help minimize changes to your diet and avoid unintentional weight loss.
Seeing a complementary care provider early can also help by establishing a baseline evaluation. This assesses how your symptoms progress and may inform aspects of future care.
HOW TO FIND COMPLEMENTARY CARE
The best ways to find complementary care support are to talk with other members of your care team, talk to the staff of the nearest movement disorder center, or ask for recommendations from a local support group. If you’re having trouble finding a provider, reach out to us by email, and we’ll be happy to help if we are familiar with providers in your area.
We often get questions from people seeking a recommendation for a speech language pathologist in their area. While one option is to seek recommendations from a physical therapy office, another excellent option is the Parkinson Voice Project, an organization that offers free group sessions with a speech language pathologist.
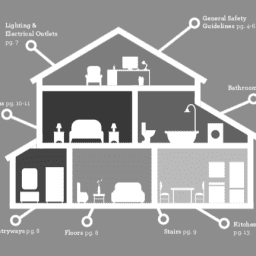
FOCUS ON HOME SAFETY PRIORITIES
We’ve covered how to make your home environment safer in multiple ways in the past, including our Home Safety Checklist, a four-part blog series, and our 2023 webinar about aging in place.
A few important ways you can your home safer include:
- Reducing tripping hazards by using automated or motion-sensor controlled lighting, installing grab bars in high-risk locations, and moving rugs out of high traffic areas.
- Avoiding use of shelves that require you to reach up or use a ladder.
- Ensuring adequate lighting around ALL stairs.
- Being careful about your furniture placement and furniture stability.
FOLLOW MEDICATION INSTRUCTIONS
There are many effective medical treatments for Parkinson’s, but all medical treatments have possible side effects. Some of these side effects—like impulse control disorders—can be dangerous for you and others in your life. Two other ways that your medications can be dangerous relate to weening off a medication when necessary and medication interactions.
The best way to minimize medication-related risks is to follow all guidance from your medical team; however, even in the best circumstances, this can be challenging. It’s impossible to know every single way your medication regimen may be thrown off, so you can’t be equipped with the answer to every medication-related question.
Moreover, you can’t ensure that difficulties related to your medication happen only when you can immediately consult with your care provider. Keep in mind that your pharmacist can be an important backup option for those moments when you can’t get in touch with your doctor.
Even with secondary options for guidance if a medication issue occurs, it’s a good idea to keep the safety information that comes with your medications so you can review it if necessary. You can also find this information for most medications online by searching online for “FDA Prescribing Information” and the medication name. If needed, consult our medication guide and our list of medications to avoid.
Avoid unnecessary risks with medications. Think critically about new treatment approaches and flashy news about Parkinson’s breakthroughs.
KEEP YOUR TEAM INFORMED ABOUT SIDE EFFECTS AND NEW SYMPTOMS
Another aspect of medication safety is keeping your care team informed of side effects. Keeping your team informed of changes can help catch medication-related issues before they become problematic.
Since it may be difficult to tell the difference between a medication side effect and a new symptom, be sure you keep your care team informed about all new symptoms you experience–especially if a new symptom seems to develop with a pattern that could be related to when you start or regularly take a medication.
PROACTIVELY PIVOT
Perhaps the most important way to minimize your risks while living with Parkinson’s is to become a master of “the pivot.”
Over time, Parkinson’s changes your abilities. The degree of these changes will vary—and you can influence these changes—but it remains critical to become aware of the evolving limits to your abilities. The key to being a master of “the pivot” is to recognize when the changes you experience start affecting your abilities and to alter your behavior before you encounter safety risks.
For example, if you notice that you stumble on the way to the bathroom at night, install better lighting and grab bars before you have a fall. Similarly, if you notice your vision is making it hard to drive at night, find other ways to facilitate transportation. Have someone else drive or leave earlier so you are off the road before dark.
The Many Ways to Pivot
The examples above are just a few ways Parkinson’s may inspire you to pivot, but there are many other opportunities to do so. For example, you are a master of pivoting when you recognize your balance is starting to become problematic when you ride your bicycle, so you shift to a trike, a stationary bike, or other mode of exercise. You are a master of pivoting when you recognize that stairs are becoming a challenge, so you rearrange your home to decrease how often you need to go up and down stairs.
To live safely with Parkinson’s, you must be proactive in assessing your circumstances and adjust your behavior—again, pivot—before a change in your abilities becomes a significant problem or causes an injury.
Keep in mind, though, that this doesn’t mean you have to give up what you love to do! Pivoting doesn’t mean stopping; it means changing directions.
AN OVERARCHING STRATEGY: KEEP YOUR SOCIAL CONNECTIONS STRONG
Each of the items above is easiest to accomplish when your social connections are strong. Maintain your relationships with friends and family, other people in your Parkinson’s community, and your care team members—including your pharmacist. Each of these people can bolster you, provide perspectives on new ways to pivot, and support your ongoing ability to live well today in unique and helpful ways.
ADDITIONAL RESOURCES
Davis Phinney Interview: All About Bikes and Pivoting to New Things
Kevin Kwok on “The Art of Mindful Pivoting”
 WANT MORE PRACTICAL ARTICLES LIKE THIS?
WANT MORE PRACTICAL ARTICLES LIKE THIS?
You can learn much more about living well with Parkinson’s today through our Every Victory Counts® suite of resources. Each manual is packed with up-to-date information about everything Parkinson’s. Click the link below to reserve your manual(s).
Thank you to our 2024 Gold Partner, AbbVie, and our Silver Partner, Mitsubishi Tanabe Pharma America, for their ongoing support of these must-have manuals. Additionally, we’d like to thank Barbara and Dale Ankenman, Abby and Ken Dawkins, Bonnie Gibbons, Irwin Narter, Lorraine and J Wilson, and Gail Gitin in loving memory of Gene Gitin for their generous donations that allow us to make these resources available and accessible to all.