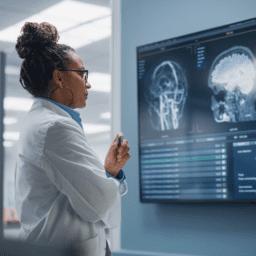
In 2012, long before healthcare had to adapt to the COVID-19 pandemic, the Davis Phinney Foundation funded one of the first studies on telemedicine and its impacts on people’s health with Parkinson’s. Nearly nine years later, its findings are more relevant than ever. The investigation became a powerful springboard for future research on telemedicine and Parkinson’s. The outcomes of the many subsequent studies can help millions of people with Parkinson’s live well today and in the future.
Here, we’ll take a look at how the 2012 study set in motion a path to more accessible care for people with Parkinson’s. To learn more about each of the studies, click the icon next to the description.
The Future of Telemedicine
Studies like those mentioned above and numerous others have now shown the effectiveness of telemedicine. Outcomes and data from the studies continue to be overwhelmingly positive, highlighting multiple benefits of telemedicine compared to in-person-care, including reduced commute time, higher patient comfort, greater convenience, increased confidentiality of services, increased access to care, a reduction in medical center transmitted illnesses, fewer missed or canceled appointments, and higher adherence to therapy.
Get Involved
One of the silver linings of the pandemic has been greater access to telehealth. However, its future is still uncertain. Congress is now deciding whether certain types of telehealth coverage should be permanent. Please consider emailing your Senators and Representatives and ask them to make telehealth rules permanent so people living with Parkinson’s can have access to providers they otherwise might not be able to see in person.
Please request and send a Red Letter to the White House and join the free “Give a Dime about Parkinson’s” Red Letter event on March 16. Hear the latest updates from host Larry Gifford, co-founder of PD Avengers, and Drs. Dorsey, Bloem, Okun, and Sherer; ask questions, and learn how to take action.
Support Our Research
At the Davis Phinney Foundation, we focus our research program on improving quality of life. Studies like RACE-PD help people with Parkinson’s live well in the immediate future. Even better, this initial study progressed to late-stage clinical research, received NIH and PCORI funding, and is becoming a therapy that is being used today by people living with Parkinson’s. You can play an essential role in this research by supporting our Quality of Life Research Fund. Click here to learn more about how your contributions help our Science Advisory Board say “yes” to more promising research projects that change people’s lives.