Welcome to the March Care Partner Meetup! During this meetup, our panelists discussed cognitive changes and helping people with Parkinson’s through them. While we don’t publish a recording of these monthly meetups because of the sensitive nature of the conversation, we want to share some key takeaways so that even if you couldn’t join us live, you can still benefit from the expertise of our panelists and community members.
Cognition Show Notes
The first symptom that comes to mind when someone says “Parkinson’s” is usually tremors. However, there is so much more to Parkinson’s than tremors, such as changes in cognition. There are a plethora of motor and non-motor symptoms that people experience. One of those symptoms is declining cognition. During this session, Dr. Mark Mapstone joined us to talk about cognitive-related issues from the perspective of a neuropsychologist, while Connie and Gail shared their personal experiences dealing with this common non-motor symptom.
What is a neuropsychologist?
A neuropsychologist is a sub-specialty-trained clinical psychologist. The point of a neuropsychologist is to understand the brain’s relationship between physical reactions to thoughts and behaviors. Adding a neuropsychologist to your team is a great way to evaluate the cognitive function of your person with Parkinson’s. Not all psychologists are certified in neuropsychology, and you cannot expect them all to be. However, having a doctor who understands that physical changes may cause mental ones as well is necessary for people with Parkinson’s.
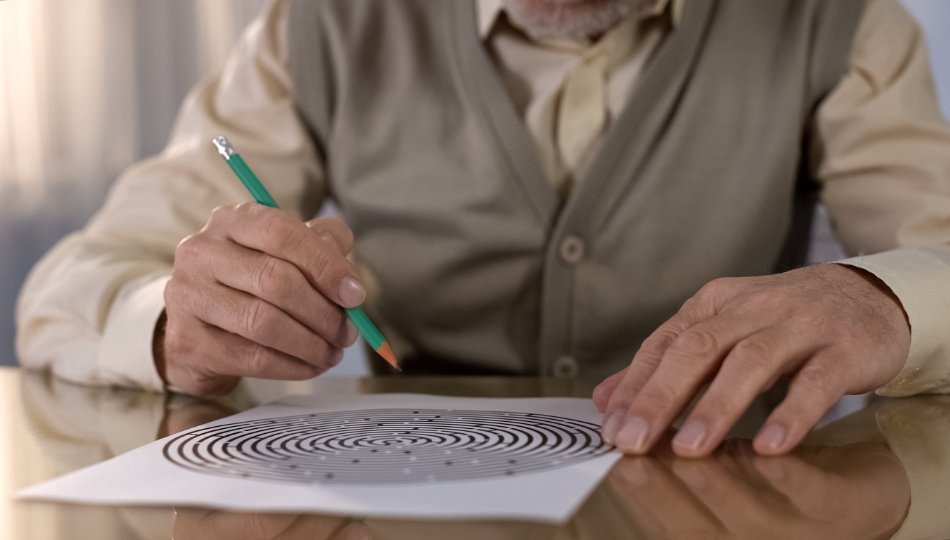
How do you know when your person with Parkinson’s needs help with DECISION-MAKING?
Cognition changes are inevitable for the majority of people with Parkinson’s. They mostly appear in the mid to late stages of Parkinson’s or at least become more noticeable at that point. Just like the death of dopamine-producing cells causes motor symptom fluctuations, so will it cause emotional and cognitive symptom fluctuation. These changes, such as mood swings or forgetfulness, may happen subtly right after diagnosis, but they typically become more prevalent as time goes on. It’s important to understand that a person with Parkinson’s has all of these symptoms combined, so issues need to be addressed holistically.
So, when do you tell a doctor if you’re noticing these issues? As soon as you see them. Just like you’d mention, “Oh, my person with Parkinson’s is having trouble sleeping,” or, “My person with Parkinson’s keeps jerking in their sleep, and it’s starting to hurt me,” you need to tell their doctor about emotional and cognitive changes as well.
Executive function changes
Let’s say your person with Parkinson’s has recently started a dopamine agonist. You notice that their decision-making has become erratic and impulsive. They say and do whatever they are thinking or feeling at the moment without considering the consequences. To learn more about some of the cognitive changes that happen as a result of medication, read this post on impulse control disorders.
Executive function is making a decision and strategizing how to execute your decision. Having executive function changes can be frightening. It’s probably also the first time you’ll notice that there are major personality changes in your person with Parkinson’s. However, what’s important to note is that it isn’t your person with Parkinson’s fault that they are making these choices. They aren’t choosing to be belligerent, forgetful, or angry. They aren’t choosing to ignore every suggestion you make (unless they did this before their Parkinson’s diagnosis. In that case, that is just them being stubborn).
The reason why these personality changes are happening is due to the frontal lobe: dopamine is produced in the frontal lobe, as are personality traits. When your frontal lobe is damaged, as it is in a Parkinson’s brain, it affects your personality as well. Gail mentioned how most of her arguments with her late husband were directly related to executive function changes, adding on to the other cognition changes. These changes are directly related to cognitive function, and it’s important to mention them to your person with Parkinson’s medical team. If a medication is helping physically but is detrimental mentally, then it may be that the medication is not actually helping your person with Parkinson’s. Creating a holistic treatment plan will improve these executive function changes and overall quality of life for your person with Parkinson’s, as well as yourself.
Symptom Fluctuations
Fluctuations in cognition are typical; there are good and bad days for everyone. Unfortunately, this uncertainty is unpredictable and difficult to deal with. There are easy-going times, and we hope and work toward those. But on days that aren’t so easy breezy, hold on and know you are not alone. When the bad days become more common, your frustration can increase. It will be shocking to see the changes in your person with Parkinson’s. Take a deep breath, accept that these changes can be scary, and remember it’s nobody’s fault.
If you don’t have a neuropsychologist nearby, what can you do?
- Telehealth: If you are not near a neuropsychologist, see if you can set up a telehealth appointment. This allows you to see them from the comfort of your own home while ensuring you still get high-quality care.
- A movement disorder specialist (MDS) is a neurologist who can do the majority of what a neuropsychologist can do. An MDS is a fellowship-trained neurologist trained specifically to understand the holistic approach your person with Parkinson’s needs. They will also be able to provide basic holistic care for certain cognitive symptoms, at the very least, so they are a great first stop.
- You may not have one locally, but it may be worth it to go the distance to find a neuropsychologist who can help. You can find a comprehensive list of neuropsychologists here.
- Go to the doctor with your person with Parkinson’s whenever possible. Use the Otter app (You can find more about it and other helpful tools here) to capture notes from your appointments. You can also ask if they understand the neuropsychological aspects of Parkinson’s as well as their movement changes, therefore seeing if finding a separate neuropsychologist is necessary.
this is a lot of information. What should I focus on first?
Of course, you should focus on the overall wellness of your person with Parkinson’s. You should also focus on your own wellness. Take time for yourself. Do the best that you can. Live with the humility of “I wasn’t perfect today, but I did the best I could”. Your person with Parkinson’s is only going to function as well as you do, so make your own health just as much of a priority as you make their health.
Additional resources
Living with and Managing Parkinson’s Disease Psychosis (Hallucinations and Delusions)
Meet Our Panelists
Mark E. Mapstone, PhD, is a licensed UCI Health clinical neuropsychologist who specializes in cognitive assessments of older adults. He has a special interest in developing strategies to maintain successful cognitive aging. A professor of neurology in the UCI School of Medicine, Mapstone has long conducted research on the early detection of neurological disease using cognitive tests and biomarkers obtained from blood. Mapstone earned a doctorate in clinical psychology at Northwestern University in Chicago, Ill. He completed fellowship training in neuropsychology and experimental therapeutics at the University of Rochester in Rochester, NY. The National Institute on Aging presented him with a Career Development Award, and his research has been funded by the National Institutes of Health. The author of more than 100 research articles and book chapters, Mapstone and fellow UCI School of Medicine researchers are spearheading an international effort to identify biomarkers of Alzheimer’s disease with a $109 million grant from the National Institutes of Health. Mapstone sees patients in Irvine and Newport Beach.
Connie is an entrepreneur, author, artist, life-long athlete and is extremely passionate about her work as a board member of the Davis Phinney Foundation. Connie particularly enjoys sharing her experiences via the written word and she is an eloquent and humorous public speaker. She has two adult children, Taylor and Kelsey, with her husband Davis Phinney.
Gail Gitin was a care partner to her husband, Gene, for more than 15 years. After many attempts to get answers, Gene was officially diagnosed with Parkinson’s by a movement disorder specialist, and he and Gail began their journey to live well with Parkinson’s. Living in Boulder helped Gail and her husband learn about and feel quickly supported by the Davis Phinney Foundation. With multiple opportunities through support groups, exercise classes, and lectures to increase understanding surrounding Parkinson’s, Gail and Gene were able to improve their quality of life and develop a positive outlook. With five grandchildren, Gail enjoys spending time with them and setting up art projects. Her perfect Sunday involves an outdoor adventure, followed by dinner at a fine restaurant and a cocktail in hand. If she’s not baking or making friends, Gail can be found at her art studio among paints and canvases!
ENJOY THIS MONTH’S CARE PARTNER MEETUP?
Join us next month on Tuesday, April 4, at 12 pm MDT. You can register here!
WANT MORE PRACTICAL ARTICLES LIKE THIS?
You can learn much more about living well with Parkinson’s today through our Every Victory Counts® suite of resources. Each manual is packed with up-to-date information about everything Parkinson’s. Click the link below to reserve your manual(s).
Thank you to our 2023 Peak Partners, Amneal, Kyowa Kirin, and Sunovion, and our Every Victory Counts Gold Sponsor, AbbVie Grants, for their ongoing support of these must-have manuals. Additionally, we’d like to thank Barbara and Dale Ankenman, Abby and Ken Dawkins, Bonnie Gibbons, Gail Gitin in loving memory of Gene Gitin, Irwin Narter, and Lorraine and J Wilson for their generous donations that allow us to make these resources available and free to all.