For many people with Parkinson's and their loved ones, swallowing difficulties are a top concern. Difficulty swallowing, or dysphagia, is extremely common in Parkinson's, with studies showing that more than 80% of people with Parkinson's will develop dysphagia at some point during their time with Parkinson's. (Note: dysphasia, also a condition some people with Parkinson's experience, relates to a speech disorder.) The good news is that several strategies can help you improve your swallowing and manage dysphagia, and the earlier you get started, the better. In this post, we'll explain the basics of dysphagia, its causes, common symptoms, complications, diagnosis, and treatment strategies so you can manage this symptom and live well with Parkinson's.
What is dysphagia?
Dysphagia is the medical term for swallowing dysfunction. Although occasional dysphagia is typically not a cause for concern, when persistent, it can lead to several health problems, most importantly choking, the inability to breathe, and aspiration pneumonia.
There are two categories of dysphagia: esophageal and oropharyngeal. Esophageal dysphagia refers to the feeling of food getting caught in the base of your throat or in your chest after you've begun to swallow. Oropharyngeal dysphagia is difficulty initiating a swallow, typically caused by structural, anatomic, or neuromuscular abnormalities. Oropharyngeal dysphagia is the category most often associated with Parkinson's. However, it can also be caused by conditions such as esophageal cancer, oropharyngeal cancer, brain or spinal cord injury, and stroke.
What are the symptoms of dysphagia?
The common symptoms of dysphagia include:
- Difficulty swallowing food, liquids, and/or pills
- Pain while swallowing
- Coughing or gagging while swallowing
- Feeling that food is stuck in your throat or chest
- Inability to swallow
- Regurgitation
- Heartburn
- Drooling
- Weight loss
- Frequent respiratory problems
What causes dysphagia?
Dysphagia can be caused when the muscles and nerves used for swallowing are damaged or weakened or when a health condition causes the back of your throat or esophagus to narrow. In Parkinson's, rigidity and bradykinesia (or slowness of movement) often cause dysphagia. These movement symptoms and the swallowing issues they can create are caused by the loss of dopamine-producing neurons in the substantia nigra area of the brain. At the same time, the loss of neurons in other areas of the brain can impact the overall control and coordination of swallowing, so dysphagia is sometimes considered a non-motor and motor symptom.
Although dysphagia can occur at any age, it's more common in older adults because natural aging and normal wear and tear on the esophagus can weaken the muscles needed for swallowing. That said, dysphagia is not considered a typical sign of aging; that fact and the fact that it's a common Parkinson's symptom mean it's essential that you speak up right away if it's a symptom you experience.
What are the risks associated with dysphagia?
For most people with Parkinson's, swallowing challenges are mild at first and may stay that way for quite some time. However, dysphagia typically gets more severe as Parkinson's progresses. No matter its severity, it can have a significant impact on your quality of life, and at any stage, if left untreated, it can cause serious complications, such as those listed below.
- Malnutrition and dehydration. If dysphagia has led you to eat and drink less, you may begin to suffer from malnutrition, unwanted weight loss, and dehydration.
- Choking. Another risk of dysphagia, choking, can be fatal if food completely blocks your airway and isn't dislodged.
- Aspiration. Persistent dysphagia increases your risk of aspiration. Aspiration happens when food or liquid enters your windpipe (trachea), and as you try to swallow, it filters into your lungs. Parkinson's and dysphagia can increase your risk for aspiration, leading to more serious problems such as aspiration pneumonia and pulmonary edema.
- Aspiration pneumonia. Pneumonia is a medical condition characterized by inflammation and infection of the lungs or large airways. Aspiration pneumonia can occur when food or liquid is breathed into the airways or lungs instead of being swallowed, and the germs from the food or drink particles infect the airways. (Watch this video of aspiration in action.) Because aspiration pneumonia is a leading cause of death in people with neurodegenerative disease and the number one cause of death in Parkinson's, you must talk with your care team about safe swallowing and dysphagia management.
- Increased Parkinson's symptoms. If dysphagia impacts your ability to take your Parkinson's medications as directed and on schedule, you may experience more OFF times and under-managed symptoms than you would if you could swallow your medications more easily.
How is dysphagia diagnosed?
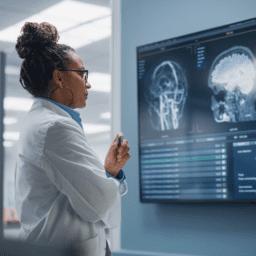
There are several tests available to help providers diagnose dysphagia. For example, a barium X-ray can help your physician study changes in the shape of your esophagus as you swallow and assess muscular activity. Another test that relies on barium is a dynamic swallowing study. For this test, you swallow barium-coated foods of different consistencies. Images are then created that show your provider how the foods travel down your throat and what complications may affect your swallow.
Your provider may also choose to do an endoscopy. In this procedure, a physician inserts a thin, flexible, lighted instrument (an endoscope) down your throat, allowing them to see your esophagus. Your provider can then take biopsies of the esophagus to look for inflammation, narrowing, or other possible causes of your swallowing difficulties.
A manometry is another type of tube that can be inserted into your esophagus. Once inside, it is connected to a pressure recorder, which measures the muscle contractions of your esophagus as you swallow.
Finally, imaging scans like CTs and MRIs can help your provider see detailed images of specific tissues and organs to make a dysphagia diagnosis.
How can I manage dysphagia?
From smaller meals to therapy and surgery, there are several strategies you can explore to help manage your dysphagia and improve your swallowing.
- Eat slowly and chew your food thoroughly. A no-cost way to improve your swallowing is to cut your food into small pieces and chew it several times before attempting to swallow. Experiment with eating several small meals a day rather than three larger meals and be sure to eat slowly and sit up straight at every meal.
- Visit a speech-language therapist. When you visit a speech-language therapist or pathologist regularly, they can help you maintain your swallowing strength (as well as your voice and communication abilities). They can also check for swallowing red flags that have occurred since your last visit so you can address any issues as soon as possible. A speech-language pathologist can also help you with expiratory muscle strength training (EMST), a key strategy in managing dysphagia (more on that below), and/or the Lee Silverman Voice Technique (LSVT), a therapy designed initially to help people with Parkinson's improve their speaking but that can also be used to help people learn to swallow safely.
- Explore expiratory muscle strength training. As mentioned above, EMST can be a powerful way to strengthen your swallowing muscles while also improving your voice and other Parkinson's-related speech challenges. Studies have found that just four weeks of EMST improves the swallowing safety of people with Parkinson's.
- Consider dietary changes. Choosing foods that are easy to swallow can help you manage dysphagia, as can techniques like blending a portion of your food and cooking foods until they are very soft. If thin liquids create swallowing problems for you, you can experiment with adding thickeners that can help. When you work with a registered dietician, especially one who understands Parkinson's well, they can help you make dietary adjustments like these that keep you well-nourished and swallowing safely.
- Ask your physician about medication adjustments. If your dysphagia makes it difficult for you to swallow your Parkinson's pills, ask your physician if there are other forms of the drug and for advice about pill-splitting and other techniques to help you take your medicine. Your physician may also be able to make changes to your prescriptions to see if a different medication helps better manage your dysphagia.
- Discuss surgical options with your care team. If your dysphagia gets so severe that you're often unable to eat and drink, your physician may recommend a feeding tube to keep you hydrated and nourished without needing to swallow food and liquids. Another tube, called a stent, may also be considered if dysphagia is severe; this tube can be inserted to help prop open your esophagus and make it easier to swallow.
Another surgical option involving a tube is esophageal dilation. In this procedure, your surgeon inserts an endoscope into your esophagus and inflates an attached balloon to stretch (or dilate) the esophagus. Other surgical treatments exist to help specific kinds of esophageal conditions, so talk with your provider if you think surgery might be a good treatment for you.
As you can see, although dysphagia is a common and serious Parkinson's symptom, you can manage it and improve your swallowing. Talk to your care team about your swallowing concerns and what treatments might be right for you.
Want to learn more about Parkinson's symptoms and treatments?
You can find much more in our Every Victory Counts® manual. It's packed with up-to-date information about everything Parkinson's. Request your free copy of the Every Victory Counts manual by clicking the button below.
Thank you to our 2022 Peak Partners, Amneal, Kyowa Kirin, Sunovion, and our Every Victory Counts Gold Sponsor AbbVie Grants, Silver Sponsor Lundbeck, and Bronze Sponsors Supernus and Theravance for helping us provide the Every Victory Counts manual to our community for free.