There is ample evidence that shows that including exercise, good nutrition, socialization, and more can help people with Parkinson’s manage their symptoms, improve mood, and live well for many years. Yet exercise, eating, and social habits look vastly different for different people, and without addressing this cultural context, accessibility barriers can keep people from integrating these practices to improve their quality of life.
In this episode
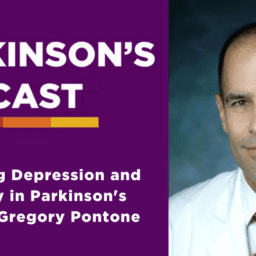
Dr. Indu Subramanian and Dr. Gregory Pontone dig into what it means to apply a cultural context to living well and how the Parkinson’s sector can implement changes to support more people in their pursuit of living well.
To download the transcript, click here.
- Historically, the cultural image of who gets Parkinson’s is predominantly that of older, Caucasian, affluent men and it’s important to begin to change the image to better reflect the true range of people that get Parkinson’s
- When prescribing ways to live well with Parkinson’s, it is important to keep in mind the unique aspects of the individual’s life including but not limited to: culture, race, location, religion, and socioeconomic status. Dr. Subramanian gives an excellent example of a patient who is told to live well by eating a variety of fruits and vegetables, but that patient lives in an area where the only accessible grocery store is a gas station
- If medical professionals increase their practice of looking at the patient from a holistic, cultural context, it will also likely increase trust between the patient and the doctor, which is often lacking in patients from certain cultural backgrounds due to history and past experience
- Understanding cultural practices and context may increase the physician’s understanding of their patient and lead to better diagnostic and prescribing practices. For example, a patient who comes into the clinic and is from a culture in which expressed emotion tends to be low, may downplay symptoms that are actually causing them great distress. If a physician is aware of this tendency, they may be better equipped to lead the conversation to address the patient’s symptoms
- The expectation to holistically assess and address a patient in the 15 minutes people usually have with their neurologist is unrealistic. So, as Indu says, it becomes the question of how can medical professionals engage a multi-disciplinary approach and recruit the community to get these holistic needs addressed
- People with Parkinson’s who struggle with non-motor symptoms such as anxiety or depression may feel embarrassed or shameful to share these symptoms with others, and this can be further exacerbated by cultural expectations or stigmas. It is important to first, recognize where the shame is coming from–whether it be from cultural practices, personal trauma, etc. Secondly, we can educate community members on the biological symptoms (including anxiety and depression) of Parkinson’s to begin to reduce the stigma and increase understanding
- Dr. Pontone and Dr. Subramanian also emphasis that community is often built through shared experiences, and finding new community among others with Parkinson’s can be extremely helpful in living well with this diagnosis
Additional Resources
Health Disparities: Structural Racism and Oppression
Health Disparities: The LGBTQ+ Community
Health Disparities: Understanding the Role of Trust
Health Disparities: The Gap Between Urban and Rural
meet the panelists
Dr. Subramanian received her medical degree from the University of Toronto, Canada. She did her neurology residency and Movement Disorders fellowship training at UCLA. Dr. Subramanian has stayed on at UCLA and is now a Clinical Professor of Neurology. She established the movement disorder clinic at the West Los Angeles Veterans Administration and has assumed the position of the Director of the Southwest PADRECC (Parkinson Disease Research, Education, and Clinical Care) Center of Excellence in Parkinson’s. She has developed a strong interest in integrative medicine with a special interest in Yoga and Mindfulness. She underwent a 200-hour yoga teacher training and studied mindfulness at the VA with J.G.Serpa and Christian Wolfe through Insight LA. She is designing a yoga teacher training program for yoga instructors who are interested in working with people with Parkinson’s. Dr. Subramanian recently got board certified in Integrative medicine. She is also passionate about palliative care in Parkinson’s. She is doing a contemplative fellowship for health care providers through the New York Zen Center and is an AAN Palitucci Fellow. She is the host of a virtual support group with world experts in Parkinson’s and co-edits a blog for people with Parkinson’s.
Dr. Pontone is an Associate Professor in the Departments of Psychiatry and Neurology at Johns Hopkins University School of Medicine in Baltimore, Maryland. He is an Attending Psychiatrist in the Geriatric and Neuropsychiatry division and is the Director of the Johns Hopkins Parkinson’s disease Neuropsychiatry Clinic, which focuses on diagnosing and treating the neuropsychiatric aspects of Parkinson’s and related disorders. Dr. Pontone’s research focuses on the interaction between neuropsychiatric symptoms such as cognitive impairment, anxiety and depression, and motor impairment in Parkinson’s. After completing a medicine internship and residency training in psychiatry at Johns Hopkins, Dr. Pontone completed a two-year fellowship in geriatric psychiatry and movement disorders focusing on Parkinson’s through the Clinical Research Program of the Morris K. Udall Parkinson’s Disease Research Center at Johns Hopkins. He also completed a fellowship in Clinical Trial Methods in Neurology sponsored by the National Institute of Neurological Disorders and Stroke. Dr. Pontone also serves on the Scientific Review Committee and as the chair of the Cognitive/Psychiatric Working Group for an international consortium of Parkinson’s disease researchers, the Parkinson Study Group.
Presented in partnership with:

Thanks for Listening!
To share your thoughts:
- Leave a note in the comment section below.
- Ask a question by emailing us here.
- Share this show on Facebook.
To help out the show:
- Leave an honest review on iTunes. Your ratings and reviews really help, and we read each one.
- Subscribe on iTunes.
Listen & Subscribe
Apple Podcasts | Stitcher
*The Third Season of the Parkinson’s Podcast is made possible through generous support in honor of Dr. Margaret Hilgartner.