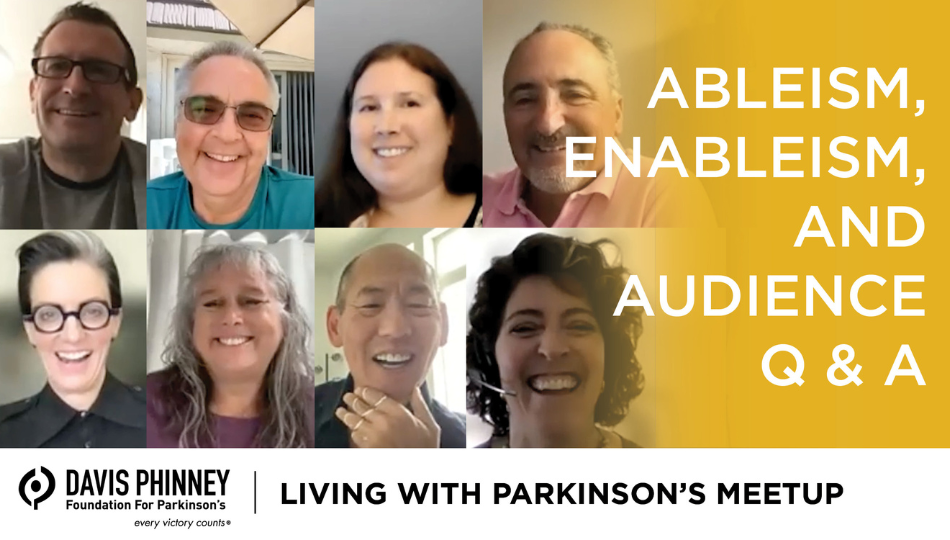
Our September Living with Parkinson's Meetup was another high-spirited event. We had three faces join us for the session, and we talked about the differences between ableism and enableism, plus a wide variety of other topics. Below, you can watch a recording of the webinar and read our show notes. Thanks to all who joined us, and we hope to see you again next month! Not registered for the meetup yet? You can do that here.
Living with Parkinson's Meetup: September 2022: Ableism, Enableism, and Audience Q & A
Read the transcript below or click here to download.
(Note: This is not a flawless, word-for-word transcript, but it’s close.)
Melani Dizon (Director of Education, Davis Phinney Foundation):
To get started, I want everybody, we have a lot of new people and I want everybody to understand who you are, so we're going to do some rapid introductions but don't feel pressure. You don't have to be super-fast if you're not a fast talker. There's no problem with that. Just say your name, how long you've been living with Parkinson's, and where you live. That's really helpful for, especially with our ambassadors. We have people that are calling in from all over and they like to connect with people who are sort of local to them. So, if you can let us know where you're calling in from. That's great. How you got involved with the Davis Phinney Foundation. Maybe your greatest challenge today of living with Parkinson's that might be different than 10 years ago when you were diagnosed and then maybe your greatest joy or surprise benefit that has come since your diagnosis. Okay. I'm just going to go around my screen here. So, Kat, you’re first up.
Kat Hill (Ambassador, Davis Phinney Foundation):
Hi everybody. I'm Kat Hill. I am currently in Champoeg Park in Oregon. I'm traveling around in an,
Melani Dizon:
The best name over, Kat.
Kat Hill:
I know. And let's see, I've had Parkinson's for eight years and I got involved with the David Spinney Foundation as an ambassador. And my biggest challenge is faulty wiring in the brain, trying to organize my thoughts and retrieve them in a timely fashion. And my probably greatest joy is all of you that are here, this community and Heather's new glasses are my greatest joy right now. they're
Melani Dizon:
So good. I feel like we need to hear about those. Yeah. Thank you, Kat. Christy?
Kristi LaMonica (Ambassador, Davis Phinney Foundation):
Hi, I'm Kristi LaMonica. I am from upstate New York. Formally I was diagnosed in 2020, but in reality, I know I have symptoms going back to like 2014. So, I got involved with the Davis Phinney Foundation. First, it started with every Victor accounts manual, which is under my coffee table downstairs. And then I just kind of being a scientist. I fell into some research projects and ended up with meeting Polly, and the WPC women's committee with Kat. And here I am involved in many ever Victor couch Chan challenges and so on. So, my biggest problem right now is OFF time. So, I'm trying to figure out how to navigate that very well. And I guess my greatest joy is the same as Kat’s, the community, you couldn't ask for a better community. I feel so supported and I have loved everybody that I meet.
Melani Dizon:
Oh, thanks. That's great, Kristi. Tom?
Tom Palizzi (Ambassador, Davis Phinney Foundation):
Hello everybody. I'm Tom Palizzi. I'm from Denver, Colorado, or just outside of Denver. And I was diagnosed in 2008, so it's been about 14 and a half years for me with Parkinson's. Let's see. How'd I get involved with the Phinney Foundation? I've just been around forever and, and I've known these folks for a long time through other, other relationships and I've just been an ambassador and whatever else I can do for 'me. Well, let's see. The biggest challenge is I don’t know, I'm starting to enter into the dyskinesia phase. And so, I'm just kind of dealing with that a little bit and that's sort of the latest of the big challenges, right? But the joy is by far in a way overwhelm and overtake all those challenges. And that joy is really helping people like yourselves and in this group here. So that's who I am.
Melani Dizon:
Thanks, Tom. Doug?
Doug Reid:
Hi everyone. I'm Doug Reid. I live in Lafayette, Colorado. I'm about seven miles from the Davis Phinney Foundation office. And I volunteer at the office a couple times a week or, at least once a week. I was diagnosed 12 and a half years ago when I was 36. And about three and a half years ago, I watched the Davis Phinney webinar on DBS and that's what hooked me on the Foundation. And I consider myself the poster child for positive outcomes of DBS surgeries. I've had a remarkable time with the DBS. My biggest challenges these days are probably apathy mixed with a little depression. And I have some of that brain fog that Kat mentioned. One of the good outcomes of having Parkinson's is that I've become a gym rat. And I spent a lot of time at the gym. And I had my annual physical recently and I'm in the best shape I've been in in years.
Melani Dizon:
That's excellent.
Doug Reid:
Deep exercising.
Melani Dizon:
That's awesome, Doug. Robynn.
Robynn Moraites (Ambassador, Davis Phinney Foundation):
Hi everybody. I'm Robynn Moraites from Charlotte, North Carolina. I've been living with Parkinson’s since my early thirties, about 2003, and then my tremor surfaced in 2013, but I was properly diagnosed at the end of 2015. You know, I can't remember how I originally learned about the Davis Phinney Foundation, but I went to the world Parkinson's Congress in 2016 in Portland, and I hung out at your booth for a really long time. And I got a manual there called every victory counts manual. And I'm going to ask Sam to throw that up in the chat, the link to that so that people know it's a manual that's free to everyone. It's really spectacular. And my biggest challenge is processing speed and organizing my thoughts when I get kind of put on the spot. It's like chickens in a coop fluttering around everywhere. And my greatest silver lining is that having Parkinson's has given me permission to tackle my bucket list now and to live my very most expansive, biggest life I possibly can. And so, carpe diem, seize the day, is my mantra. Thanks.
Melani Dizon:
Thanks, Robynn. That's fabulous. Heather?
Heather Kennedy (Council Member, Living with Parkinson’s Meetup):
I like that, carpe diem, seize the day. It's probably better than memento Mori, which means remember you'll die, but that's, we, him, you know, we're going to live.
Robynn Moraites:
You got to keep it real, man, got to keep it real.
Heather Kennedy:
Let's live now while we can right here together. That's my-
Tom Palizzi:
Do the carpe diem first.
Heather Kennedy:
Yeah. Right. So, Heather Kennedy, I love working with this organization because it's vibrant, it's real, it's authentic and fun. And as an added bonus, when you're stuck somewhere, they really try to help, and they care. And I just want to thank the Davis Phinney organization for that. And all these people here, my friends who, who come to my rescue and love me when I wasn't very lovable, which I think is my greatest joy to get that unconditional love is like so amazing. You know, like when we screw up and people still say, you know, it's okay, you're human. You're going to screw up. It's okay. So, thanks for letting me join you today. And I just, I write as Kathleen Kiddo, and I try to do as much volunteer work as I can. So, thanks.
Melani Dizon:
Thank you, Heather. Brian. Hello.
Brian Reedy (Ambassador, Davis Phinney Foundation)::
Hi. I'm Brian Reedy. I live in Southern California around Huntington Beach. I was diagnosed in 2010. I first learned about the Davis Phinney Foundation when I went to their conference in Las Vegas. And I credit that with changing my life with Parkinson's because for the four or five years before that I was almost outate a Walker and wasn't moving very well at all. And then they started talking about extensive exercise and riding bikes and what nobody in my area was talking like that. And then we found a physical therapist who could do that type of physical therapy and changed better since then. So, when they started the ambassador program and I heard about it, I jumped on it because it's like, want to keep singing the praises that I learned from. I'd say my biggest challenges are movement and depression movement.
Because I had a bad truck accident a few months ago and it hurt everything head to toe. And so that challenges my Parkinson's considerably. But that's also my greatest joy is the more I move the better I feel. So, I don't let the pain win. I seek out the victories in, in doing things and I'd add to that the community because when, when I'm down and challenged, many of the people on this panel and many of the people within the Foundation I can talk to and their family and, and that's really the support you need through a support group or through the Foundation itself or whatever. But it's when you have that kind of considered loyalty, I guess, where, where they just are so honest and open with you and, and therefore you, when nobody else seems like they will be. That's the greatest thing about the Parkinson's community, I think.
Melani Dizon:
Yeah. Thank you, Brian. And welcome. And last but not least, Kevin.
Kevin Kwok (Ambassador, Davis Phinney Foundation):
Hey, is my speaker on?
Melani Dizon:
Yeah, we can hear you.
Kevin Kwok:
Hi everyone. I'm Kevin Kwok. I know most of the panel here. So, this, as Brian was saying, you guys are my family and I love these family gatherings. I've been living with Parkinson's now for 13 glorious years, each year has been exciting and interesting with lots of new challenges. came first to the Davis Phinney Foundation when my neurologist said Davis was supposed to be on a panel here, but he can't make it. Can you suffer him? I had no idea who he was at the time. And so, I called Davis and I said, Davis, I really can suffer you if I don't know you. So, we had a two-week session where every morning where I commuted to work, I called him, and we just chatted. Those were two glorious weeks of really getting to know someone and subsequently, they invited me to join the board, which has completely changed my mind.
I actually moved here to Boulder to be close to the Foundation. And every day I worked with you all, I learned something new. I gained something new, and I think my life gets a bit more enriched. What I'm dealing with today, which is probably my biggest challenge is accepting the fact that I'm entering the next stage of Parkinson’s the days of, of just mu musing through and, and sort of Pollyannaish sort of rah, you know, you can beat this thing now is subjected to more of symptoms, linger a little longer. They're a little harder, and it's just the next phase. But those days of just out Ling, the disease have sort of come now tomorrow of, of this next phase of just having to negotiate and deal with it. It's not worse, but it's definitely there. And I think that as all of us advance in our disease journey, we'll have to learn how to get here and sort through it. So, I'm looking to all of you to help me get through.
Melani Dizon:
Thank you, Kevin. I think, yeah, you got a lot of head nods with that one. So, I think there's a lot of people on the panel who are appreciating that and recognizing that. So, I would love, while we can't see and hear any of our audience members, I would love it. If you are open to it, putting in the chat, just the first thing, put your greatest challenge today, comma your greatest joy. It would just be nice for all of us to get a sense of what you're dealing with too. And I also got a lot of questions coming into my email and please know one of the things that I know, I can't remember who said it, oh, I think it was Brian. I can't think and talk at the same time. I hope I'm not the only one who can't do that.
I put blog@dpf.org. As Brian said, you know, feeling like you have somebody to talk to, I still get emails from people. And when I respond, they're still surprised I respond. But we do respond. That's one of the things that we take really seriously at the Davis Phinney Foundation. So, if you have a question or you need a resource or anything just email us, and we will figure it out. And if we don't have the answer, we will find it in somebody else. Okay. So same as Kevin, the journey trying to leave each life each day, as best I can, balance is an issue. Joy is to feel grateful. Excellent. As a care partner. My biggest challenge is watching my dad enter that next stage. Yeah. So, my biggest joy is that I get to work here at the Davis Phinney Foundation and learn alongside all of you. Challenge: Aging with Parkinson's, yes. Challenge, anxiety about the future. I think that's such a big one. Gosh. Right? A great joy includes how much better I feel after taking my medicine. Yes. motivation ability to swim again after starting meds. Yeah. That's so great. You know, a lot of people will ask us when is a good time to start taking medication and people say, actually, Kat, can you finish that? Because I'm about to have a coughing fit. Can you finish that sentence?
Kat Hill:
You bet. So is, is when you're ready. And when you feel like your symptoms are getting to the point that it's impacting your life. And so, and I think it's also a really, really individual choice for people. So, and it's one that needs to be made in tandem with your provider. But I wish I would've started meds sooner than I did. I waited a long time because I was worried about side effects, and I just felt, feel so much better on them. So
Melani Dizon:
Thank you, KAT you bet. Team effort. Okay. so, thank you, everybody. Patience, decompressing in Colorado. Excellent. I'm going to start out with one of the topics and I'm going to let Heather and or Kevin present it. And this is the idea of ableism and enables, I'd love for you guys to present the topic and talk a little bit about what that means to you, and how you came to start discussing it. And what do you think is important for everyone on this panel to consider and think about Heather, want to go for it?
Heather Kennedy:
I have to give some credit to somebody for this for these phrases Kat Hill has been talking about this ableism versus enables. So has Kevin quite a bit. Kevin mentioned it. In fact, in some writing, he gave me, it's the difference between making things a little bit easier and acting really put out and making things a little bit harder for someone who has at varying stages of disability. One of the greatest examples that I can think of right now is I could not move through a doorway simultaneously pulling my luggage and getting through the doorway and closing the door and I couldn't get any help for whatever reason, nobody in this hotel would help. And I just couldn't get anybody to listen. And I even said, I'm in the handicapped room, I'm in a special room here, you know, can any, they wouldn't send somebody.
They wouldn't believe me. That was you know, really difficult. So that made my disability worse. But when you enable somebody and give them it, it's the opposite of what, how, and how you use this term in psychological terms. Like you're not enabling them to have bad behavior. You're enabling them to, to be able to be independent if they'd come up and just simply held the door open, I could have pulled my luggage through and walked through. And none of that would've happened. It would've been so simple with someone who could walk and, you know, had their physicality about them. But that OFF time, like Kristi mentioned, many people mentioned in the thread is what throws everybody. So, I think this, even if we don't understand Parkinson's or whatever people are dealing with, we don't know what people are dealing with to enable them to help them. Like, for example, would you like some help crossing the street? No. Okay. I'm still going to walk near you, is that okay? Crosses and you know, it's just enabling them. And then this, this, this disability, we can become more disabled when we are in stressful situations where nobody gets it. We feel very much alone. Like that example I just gave. What do you think, Kevin?
Kevin Kwok:
Yeah, I sort of this, this topic of ableism and enables is something that's been kind of on my mind quite a bit, you know, I always wonder what ableism is, right. And you know, there's the dictionary definition where it's prejudice against people who cannot do something because of a disability. Well, that, there's, that's a very rich definition because it means one at first you have to admit that you have a disability. And so, for so many of us who go through the early stages of Parkinson's, we don't allow people to help us because we want to just sort of either deny it or blast through it. So, part of the, and this lends to a question, I think that someone sent in on, on just predictability, well understanding that we don't have a predictable disease is part of that understanding and admission. So, part of ableism is, is, is getting comfortable with, with this term, are we disabled ourselves?
It's not an easy term to accept. But my view on this is that people and we experience ableism both in a corporate sense and in a personal way, people, your family, and friends, sometimes unconsciously practice, ableism, and companies do that. Your employers can do that and your colleagues as well. And it's never really deliberate, but it hurts. And I think coming to this understanding that it's not deliberate, it's not conscious allows you then to think about the converse and that is what would you like to have? And that's, so that brings on the enables side for me. And so, I think this is a topic that, or Heather, you just mentioned it, it's picking people out so that they can do it themselves versus just taking it away from them, thinking that that's a burden to them. It's something that I'm struggling with right now, of accepting help so that I can get things., I don't mean to run on a rant on this, but I think we could spend an entire hour talking about this concept of ableism and the converse enable. I'm curious if others on our panel think this similar or what their thoughts are,
Kat Hill:
Just raise your hand or a Kat. Yeah. And then tell I'll jump in. I think part of what can be difficult for the people who love and care for us are that our symptoms are unpredictable and they're not consistent. It's frustrating for us. And I think it can be frustrating for them. And so, I think kind of I'm back to the, my, my harping on communication and, and me being able to say things like it's really getting difficult for me doing X, Y, or Z, you know, opening cans, you know, of a can opener or chopping things, Kevin, you, and I both get that the hand thing. But what I'd like to do, if you're okay with it, honey, Ken, my husband, I'd like to be able to ask, rather than you are jumping in and just automatically doing it because when it's taken away I feel more disabled.
I'd rather be able to say, honey, I'd love some help with this. Or how about I do the sauté while you do the chopping or whatever. And we've learned that dance, I suspect we're going to learn it over and over and over again, as things get more and more difficult. And, and I also think we need to empower the people that love and care for us, our coworkers, those to ask questions. And the phrase that I like is how can I best support you? Because it's not saying, how can I do that for you? How can I take that away? And I'm not offended by that part. You know, here, let me do that. Doesn't feel as good as how, how can I support you right now? Those are just tools that are working for me right now.
Melani Dizon:
Love that.
Tom Palizzi
When they say it's, when they say move, step outate the way that doesn't have. I think that that's definitely the case, you know, that this whole notion of discrimination that favors able-bodied people is what, what ableism is. And I think it, you might think of that more in terms of a professional, our corporate world, but getting, getting more in our personal lives. I mean, it definitely comes up, but I think what's helped me deal with that and manage that is just pure honesty. I talked, I told everyone, I knew when I, well, not everyone I knew, but I told everyone that was important to me when I was diagnosed. And that helped set the stage for where I'd be going. And then as the kids grew up, not my kids, but my nieces and nephews I'd tell them. And so, they always knew how to see me, not necessarily get, be surprised by what would happen.
So, and, and then a little bit of humor, I think always helps that. So, I, we were in a bike ride myself and my buddies and I got, I got a flat tire. And so, I hop off the bike and, and I'm starting to repair my tire and they're all waiting there, you know, twiddling their thumbs, waiting there, and waiting there. I, one of 'me goes, look, this is not the time for a personal victory. Get outate the way. So, it's just those kinds of that kind of humor you throw into the situation. And that always helps. So that's, that's a fond way to look at it. So yeah, I think enables comes then from that viewpoint into more of a communicating with your loved ones, your friends, whatever, my family here, like Kat said, and just you know, ex explaining to them how you'd like to deal with stuff or what may work better for you and what may work better for them.
Melani Dizon:
Thank you, Tom. Kristi?
Kristi LaMonica:
I've actually turned a lot better around. And so, teach I'm a college professor and I go around to a lot of different classes, and I talked to different classes and teach students, like, how would you like to be what to say to someone when you find out that they have a disease or a chronic disease, now get better soon. That's not, that's not the appropriate thing to say. So, we talk about like Kat, where you're saying, how can I best help you? How can I best support you? What can I do? And I think that that's the best way to do it. I also to a student recently in one of my lab classes, she's lacking part of her arm and she was asking, do you think there's something I can't do? I said, no. What do you think that you can't do? I'm not going to limit you. You're going to tell me what you need, and I will best support you throughout the semester. So, I think that I'm trying to kind of spread this to everyone in my, in my classes, in my environment to best deal with people that have all sorts of disabilities and make them feel able. Because we can do it,
Melani Dizon:
Love that. I just want to share this because I think it's related and then Robynn, but Sarah says, I think a big challenge, many of us face is being okay. Letting our symptoms show that that's part of this. Right. did any of you on the panel feel this way at one time and how did you overcome this? Robynn goes. Why don't you say what you were going to say? And then
Robynn Moraites:
I was going to respond to Sarah's question. Hi Sarah. Nice to see you again. We participated together one time in another event. But that's been my issue completely. Nobody knows I'm disabled because I loved, I wrote muscling throughout muscling. That's what Kevin said and that's what I try to do. And in fact, you know, I have been telling people about my condition because I'm to the point where I really can't do public speaking anymore and it's an integral part of my job. And when I get up in front of an audience, if I even have a little bit of a tremor, I get really self-conscious about it, which creates more of a tremor than I get more self-conscious and it's just this cycling loop. And so, a lot of people I can just say, I mean, I'm happy to do presentations by zoom or WebEx. And I sort of tell people, hey, you know, I'm not traveling as much, but some people I'm close enough with that. I just say this is why I'm not doing it anymore. But Sarah, I really identified with that because I still very much try to keep my symptoms under wraps. I just I'm too vain. I don’t, there's no other way about it. And I just, you know, I know that the day will come when I'm not able to keep it under wraps, but that's where I am today.
Melani Dizon:
Yeah. I actually think that's an interesting question. I wonder if Kevin, maybe this is something that you could speak to because every, I think everyone on this panel really related to this idea of, I used to, I used to be able to get on no one knew I used to be able to do all of these things and I could hide it. I could do whatever I needed to do, and it does, it comes up right. And, and, and you're not going to be able to do anything about it. You're not going to be able to muscle through it anymore. So those are some of the challenges that Kevin talked about and would love to know a little bit about some of the ways that you're managing that Kevin,
Kevin Kwok:
You know, the bigger issue is there's some, so many of our symptoms are not detectable visually, you know, it's like, you know, NOH or loss of voice or things. And that's the tricky thing is explaining to people the symptoms they can't see. That's my bigger struggle. had a situation last week where I was invited to fly, to speak to a group of pharmaceutical executives. And my voice had gone to hell. I mean, I literally got up and had this squeaky little faint voice, and rather than try to fight through it, I apologized to the audience in advance. And I explained to them that this is one of my symptoms that you can't see, you may not know about. I ended up getting a standing ovation. It brought tears to my eyes when I finished. And they said, you know, by, by coming to us, struggling with your voice, but still trying to talk to us, we got your pain and we felt it. And they said you were more authentic because of it. That was a great learning opportunity for me, you know, and there is, is to express yourself, tell people what your difficulty is, and don't be afraid.
Melani Dizon:
Thank you, Kevin. Yeah, Doug. And then Brian.
Doug Reid:
For years, I worked in healthcare sales and made regular presentations to healthcare executives. And when I first was diagnosed, I would try and hide my tremor. But then after taking carbidopa leave dopa for a couple years, I became so disconnected that it was obvious that I had something going on when I would walk in, and I'd be a little nervous and I'd get even more disc. And I noticed when I would speak, I would become even more disconnected. So, I was very open, and I would start my presentations with, thank you for having me here a bit about me. I have Parkinson's disease. And because there were healthcare executives there, I think they knew a little bit more about it maybe than your average person does. But through, except for when I was initially diagnosed and thought I could hide things at this point, I'm very open about it. And I want to talk about people. I want them to know what's going on with me and I want to create awareness of the disease.
Melani Dizon:
Thank you, Brian.
Brian Reedy:
Yeah, I agree with that and create awareness. And when I went through a couple years before I wasn't and I was a high school teacher and there was a lot of gossip going around that, oh, he's got something really bad. He's probably dying or just, you know, a bunch of crap. As soon as I got the diagnosis, I got up in front of the staff on the first day of school. And I just said, I've got Parkinson's disease. This is what it is, but this is not going to limit me as this and this. And then I just cut jokes left and right. And the staff came up to me and number many number members of the staff came up afterward and said, you know, that's the best way to approach this thing. And then I did that with my students.
I made jokes because I had I'm in front of the classroom and I get a leg tremor that just it's vibrating the whole room. And I just make jokes about it, and we'd move on. And I tell the kids, if they'd made a really good joke, I'd give them extra credit, which went too far because their jokes were really bad, but you just incorporate it into your living and you find more joy. I think in working with it than hiding it and having the stories go the other way. So, I find the openness really worked for me and I was able to teach for three more years, and I had tremendous support.
Melani Dizon:
Yeah, I think it's great. And I think just like everything right? You, you, you learn to read the room, you, you learn to read your group, your community and say, is this going to, hey, is this going to hurt me? Is this going to help me? Like, and it, and unfortunately we live in a world where it doesn't help everybody to come out with it and say, here's the deal here. I am. It doesn't help everybody. And so, I think in those situations where you're struggling and you're wondering about finding an ambassador, reaching out to somebody on the panel, reaching out to somebody else, who's gone through it to talk about it with, you know, maybe role, play it a little bit, do something. Again, not one thing's going to work for everybody, but it is nice to know that there are people out there, there are warm, wonderful, amazing people who hear that news and treat you with the respect and love that you should get. And, and unfortunately, there are, there are people that don't. And so how do we deal with that? Christy, did you have something that you wanted to add to
Kristi LaMonica:
This? Yeah, I just want to add, so Brian, like you I've told everyone I work with because on the college campus I felt pretty safe, and I can use this to help train the next group of PTs coming forward and the next group of OTs going forward. So, I go to all their classes, and I tell them prodromal symptoms. I had, so look at patient shoes. So, I'm using it the best I can to educate everyone around me about what I have because you can't hide it from a bunch of health science people. They diagnosed me before I was diagnosed.
Melani Dizon:
Yeah. This is great. From Patty, I spoke at an EMS conference last weekend. My voice was marginal because of my burning mouth syndrome. I practiced my presentation with Dan my husband and there were a few times when he just carried on for me. Wow. That's an amazing partner. we all have a sidekick with this. That'd be pretty great. But oh Dan, that's a really great, that's a great strategy, right? yeah. Dan is quite an amazing care partner. So, yay Dan. Good job. So, one of the questions that I got really dovetails well with this, and I think this is something that y'all are going to be able to respond to. So, someone wrote in and said when you're feeling strong and you feel like you have control of everything and then you find out you don't, what do you do with that anger and that sadness? What do you do with it?
Kat Hill:
Chocolate ice cream.
Melani Dizon:
Waiting for that peanut
Kat Hill:
M and Ms. It's part of the human experience, you know, it's, I don't think it's unique to people with Parkinson's. I mean, there were plenty of times, you know, it's, it sucks it just does. And, and darn, and let's be sad and angry, and then let's move on, you know, then let's get over the hump and go back at it. I don't know. I don't have any magic answers to that one because it's yeah. It's just all a big rollercoaster ride, right. For all of us. So,
Robynn Moraites:
And was going to T on to that there's no way out, but through denying the feelings, doesn't make them go away and so, you know, when they come up for me, when they come up, I just feel them if I'm an appropriate place to feel them. And I, this is a funny story. One night, a few months ago, I was having a real problem with the coordination of my fingers, and I dropped my cooking utensil or my knife or whatever it was. And my partner has never seen me do this. I picked it up all the floor and I threw it across the room into the sink. And I screamed the only expletive that works in that situation, which is a four-letter word that starts with F, and now had you been a fly on the wall? I mean, Bill was like, oh my God, I was just so frustrated.
And I had a good laugh about it. I told my neurologist and we just started cracking up, but you know, every now and then it's just like, let it go through you. I think the more you repress it, that's when it starts to lead to non-Parkinson’s related depression like normal people get depression by trying to suppress their feelings. So, I just try to experience it, move through it, and move on. And I love what Kat said about it's part of the human experience and everybody is going through some version of something as they age in their life with all kinds of life experiences. It just happens to be the one we're going through. Thanks. Yeah.
Melani Dizon:
Thanks, Robynn. I, one quick thing and then Kevin, and then Tom one of the best pieces of advice I got, and I don't always follow it, so I'm not pretending like I know what I'm doing, but was give yourself a timer, set the timer for you're allowed to be mad for five minutes. You're allowed to be, you know, mad and rant for 10 minutes. The timer goes off, done over, move on. It's not yours anymore. And it's actually really helpful when I remember to do it. So, but that again, that's a human thing, right? This isn't something that's stressed for people with Parkinson's. So, thank you for that. Okay. Kevin and then Doug, I think, or Tom, and then Doug
Kevin Kwok:
One, one of the things that I learned a great lesson from where my old martial arts instructors, you know, they, they used to say things to me that I would never really understand until five, 10 years later, but the one thing they once told me was in order to be a great practitioner of karate, you must first learn to lose control in order to gain control. And that's something that really at the time when they said that I was like, yeah, yeah, yeah, okay. I get it. But it's taken me years to really understand that losing control the gain control. And I think that this art of ultimately relinquishing control is actually our, a way that we can come to grips with our, our Parkinson's even better. I mean, I apply this mostly to sports, you know, I'm a very stiff skier, and they said, you got to let go and just let it happen. I find that the same way in the professional world, I used to be a controller that wanted to control everything. But in order to when you do that, you somehow miss out on things. So, to answer that question, if you can just sort of accept the fact that control is no longer your realm, you might actually find that it's very relieving and enough that confusion thought.
Melani Dizon:
Thanks, Kevin. Tom?
Tom Palizzi
Yeah, that's good, Kevin. I recall Davis said once, "living with Parkinson's takes courage, and living well with Parkinson's takes that much more." And I thought about that, especially the other day, I got an email from somebody who wrote in through the website and a woman was talking about how she's had Parkinson's for quite a while. And though recently she said, I'm scared. And she was scared about not knowing her future. And she wanted to know if she could talk sometime. I said, sure. When I responded back to her, I invited all the other Colorado-based ambassadors, to comment. And the comments flooded through about her bravery and her courage to reach out to us. I thought, you know, that's really, that's really an enabling thing. So, you know, I guess the message that I always send to people from this site and this pulpit is reach out, ask us for help. We're here to help you, all of us in this group. And I'm sure everybody else. So just thought that tied in nicely with what we talked about here so far.
Melani Dizon:
Love that, Tom. Thank you. And thank you for doing that, for pursuing road in. Okay, Doug, and then Heather
Doug Reid:
Heather can go first. She had a hand raised.
Heather Kennedy:
You. Go ahead, Doug. I want to hear what you have to say.
Tom Palizzi
How do you make your hands go up like
Melani Dizon:
That? There's a little guy that says reactions.
Tom Palizzi
Okay. Thank you.
Doug Reid:
I was just going to echo a little bit when Kat said about chocolate ice cream, when something gets me down, I immediately try to do something that I enjoy. That makes me happy. Whether it's going on YouTube and finding a clip from a comedian that I know will make me laugh. But I also try to remember my gratitude and the things that I'm grateful for life can always be a heck of a lot worse than it is. And it just kind of keeps me grounded and keeps me centered.
Melani Dizon:
Thank you, Doug. Heather?
Heather Kennedy:
Yeah, like rule 62. Hey, so I was thinking about service and support, but before I get there, I have to box it out. I have to scream and stomp and get mercurial, and I'm going to throw everybody into the volcano. Everybody gets to burn because you know, I'm upset because of Parkinson's and poor me. And I go through this whole thing. It's kind of like the first thing that I do is like a volcano, throwing people into a volcano, and the second thing that I do is, you know, oh, maybe I overreact just a little. And the third thing I do is I go, wow, it's not about me. We have a bigger thing at play here. We're together for the amazing thing that we're doing, to sort of just bring information and the best way we know how we're all doing the best we can with whatever resources we have. So, and like someone just said here, things can be a lot worse. Isn’t that the truth? I had a party when I found out it was Parkinson's it could have been MS, ALS I mean, there are so many other things. And when you have this disease, lastly, we find out what everybody else is suffering from. We get to hear it, whether we like it or not, but what's cool about that is we're not alone. And here we are again, you know, I just, I don’t even know if I answered the question. I got so excited to be here.
Melani Dizon:
You did.
Doug Reid:
What is rule 62 from?
Heather Kennedy:
Oh, it's about not taking ourselves too seriously. It's from a, it's from another book.
Doug Reid:
Oh, okay.
I just love it, joking.
Kat Hill:
And I probably would call it, like, rule, you know, 6.2 or something. I almost always get it right. But not quite right.
Heather Kennedy:
Yeah. Just like let's have some fun, you know? Yeah.
Melani Dizon:
Kevin, were you, did you have your hand, were you raising your hand or no?
Kevin Kwok:
No. I was just scratching my head.
Melani Dizon:
Okay. So, I want to take a couple of minutes here and let's see, need to accept that life, that like other life challenges, you will have relatives or friends who cannot cope or still be able to accompany you through life, give them and move on. Yes. Okay. What book has rule 62 in it?
Heather Kennedy:
May I, this is a reference to recovery. Oh, I'm in recovery. So just to put it out there that just simply means in my case, I don't drink alcohol anymore because it doesn't go well with my meds, and it never ends up well for me.
Melani Dizon:
Yeah. So, okay. So, I'm going to we have a bunch of questions that came in and I want to just kind of honor the people who wrote in questions and I just want to, we'll do some rapid fire and then also people who have other questions can throw them in the chat. So, a lot of these are just some, a couple of comments and then some, some of them are just really practical questions that maybe one or two of you have an idea of, of what you could do. I do want to say that I'm not going, yes, that is actually one of the questions. I'm going to ask Kevin, but I do want to mention that we're not going to answer any of the medication questions just because it's just such a big thing. And nobody on this panel has the authority or experience or doctor next to their name to be able to answer these questions. So, I appreciate them, and I know it's frustrating if you can't get your answers from your doctors, but make sure you get the answers from your doctors. Those are the people who are going to know about the medication the most. Alright, first question. It goes to Kevin, what do you have on your fingers? And can you explain what they're for and how long you've been using them, do they work and where can you get them? If people, if you do like them and they're working,
Kevin Kwok:
It's just bling that I wear to be cool.
Melani Dizon:
Right? That's awesome.
Heather Kennedy:
So well ably.
Kevin Kwok:
No, I've had, so I actually have things on different fingers for different things, but I'll focus on the, on the finger splints because, in the last year have had really bad dystonia kick in so bad. The fact that my hands are, are truly disfigured and, and dysfunctional now a lot of the things that I like to do, like shift gears or hold a break on a bike, I can because I can't grab. And so, what my occupational therapist said, and she is doing, is fitting me with these splints to try to force these tendons back into place it's palliative. And it doesn't really seem to be working. It's not a cure. But my kids think it's a cool look. So, keep on wearing them in the meantime.
Melani Dizon:
Yeah. I mean, exactly. Heather, nobody wants to be around that. Okay. This is an interesting one for people who are dyskinetic and have that as one of their symptoms. How do you deal with dyskinesia when you're at the dentist?
Heather Kennedy:
Can Burnett, oh man. that's great. Great question.
Melani Dizon:
Anybody.
Tom Palizzi
I wish I knew that.
Kristi LaMonica:
What about just talking to your dentist and telling them? So, I always tell every healthcare provider, if they have to be doing something on me that listen, I have Parkinson's, I can't guarantee I'm going to be able to be still because it could be dyskinesia. It could be, God knows what, you know, mm-hmm, whatever else is happening that day. So, a lot of times they're very understanding
Kat Hill:
Last week at the mammogram. Okay. I'm just not going to say anything else about it. She was delightful. I wasn't disconnected, but I was so tremor, you know, that's all I can do. Yeah.
Melani Dizon:
All you can do. Let's see. Does anybody have any suggestions about special cushions to help, to find, to make sleeping more comfortable? Do people use body pillows? You know, like maybe pregnancy pillows? Is it, does anybody have anything that helps them sleep and,
Tom Palizzi
Well, I've tried everything. I think there, have a small pillow that I put, like between my knees to separate, and that helps a lot. Somebody I thought was on this group, said something about putting a bar of soap in your bed. I don’t know if you've ever heard that, but ivory or not. What is it?
Kristi LaMonica:
The restless legs, right?
Tom Palizzi
It's the lavender soap and that helps that's supposed, lavender's supposed to help.
Melani Dizon:
What is
Kristi LaMonica:
It's rest,
Tom Palizzi
Restless leg and just being uncomfortable. So, and then there's also got some padding that I added to the existing padding that's in our, in our bed. And that helped me a lot too. So just try whatever you can.
Melani Dizon:
Good. Somebody said airplane pillow for head, especially after DBS. That's interesting. Has anyone tried that airplane pillow, that's actually a great idea, right. Said, yes. What about dyskinesia and getting a pedicure
That is tough. That's got to be an ON activity only. Right.
Tom Palizzi
Here we're laughing, you know?
Melani Dizon:
Yeah. Has this is a, I mean, this is such a big topic and don’t know that we can't get fully deep into it. Because I think it's a bigger one. But advice on determining when to stop driving, has there, is there anybody on the panel who has, you know, whether you've decided I'm not driving at all anymore or there are just times when you're like, I'm not going to drive and what are the, what are the sort of telltale signs? And do you have any bright lines that, or that you have a care partner or somebody that says Nope, not doing it, Kevin?
Kevin Kwok:
Yeah. You know, what would, my girlfriend's here in town. We sometimes split. She knows that I can drive half there halfway, and then she usually drives back that that's sort of the unspoken role and don’t drink anymore and drive, I think that's a real formula for, for disaster on there. I'm going to be really sad the day that I lose, you know, the ability to drive, but I think it's just somewhat inevitable that it will eventually happen. Yeah, there are ways to be tested if you really want that, but mm-hmm
Melani Dizon:
Yeah. Sam, actually a good post about the testing. You can throw that up there if you want.
Kevin Kwok:
Do be careful because if you sort of go out of the recommendation and it's documented in your file, think from the lawyer's perspective, I'll be curious to hear Robynn’s view on this. If there's document documentation that you shouldn't be driving, don’t know necessarily if you want it out there. Right, right.
Robynn Moraites:
I agree.
Melani Dizon:
Yeah. Heather, you have a hand raised.
Heather Kennedy:
Yeah, I got so involved in answering questions, but I forgot what the question was. Oh, okay. I'm going to blame it on Parkinson's okay. Brain fog.
Melani Dizon:
Totally fair.
Heather Kennedy:
So, the question is-
Melani Dizon:
That leads me to my next question. Perfect segue. Maybe you want to answer it. Why does it feel like my brain never turns off? It's always racing
Heather Kennedy:
Because the ego needs a job
Melani Dizon:
Does-
Heather Kennedy:
Even when you're meditating, people say just clear your mind, relax, and sit there and just breathe. Right. You know, I mean, let's face it. We are always creating stories, tripping about the past, tripping about the future, tripping about something anxiety that we encounter is both causal and chemical. So, it's very real anxiety. You're not going crazy. It's actually ramping up because of Parkinson's itself. And then you recognize it's going to take you an hour longer to get out, to get out of the house today. I spent an hour trying to button this shirt, but I was taking a page out of Kevin's book when he said, it's his last act of defiance to where the button flies’ jeans I'm doing it. the point is we have, we have a million reasons to have our minds go, woo. And if you don't practice any kind of meditation or any kind of breathing exercises or calming techniques, you will find yourself in the position of go or be dragged, because it's going to get worse. And you can only take so many supplements before you're asleep or rather medication for your sleep. Right. I do find that it's helpful to say things sometimes, but sometimes talking about it makes it worse. Maybe muddy water, let stand, get still. There are a million reasons to be upset. I mean, turn on the news. Yeah. You know, you know, there's a million things going on. We feel powerless increasingly powerless. So anyway, that's my take on that and just try to have compassion for each other or try to relate to each other.
Tom Palizzi
I'll always try to recount things that I've done in my past. Remember things. It helps my memory of course, but just recounting just certain situations that had a good time or whatever, just trying to put those pieces back together. That's always kind of interesting.
Melani Dizon:
Yeah. That's a great-
Tom Palizzi
Usually puts me right to sleep. So-
Melani Dizon:
Right. Just a kind of harness, the craziness of the mind into like one memory that you're like can read it, think about it.
Tom Palizzi
And I was a boring guy, so it makes it really crazy.
Melani Dizon:
I find that hard to believe. Never.
Kat Hill:
I just also want to say, I know that when I was on the agonists, I had much more trouble sleeping and I had some other side effects with them once I shifted off of the agonists. It helped my sleep some not all the time, but I think it may also be something that you may want to try tweaking with your provider about meds that might help if you have that option.
Melani Dizon:
Kristi?
Kristi LaMonica:
I want to support what Kat just said. I have incredibly terrible restless slides at night. And if I don't take my meds at the right time, it's almost painful. I thought I was going to cry the other night because I just took my meds a little bit too late. And it just, it was painful until I take more Carbidopa Levodopa. I'm just as stuck in pain. So, I would really recommend talking to your doctor about ways to get better sleep. Because it's so incredibly important because you just feel so much better overall when you can sleep. I had forgotten what it was like to get a reasonable night's sleep until a few weeks ago. And it was like glorious. I felt like a brand-new person.
Melani Dizon:
Like I can conquer the world. Yeah.
Kristi LaMonica:
Right.
Melani Dizon:
Did somebody say something about a yoga blanket? And if yes, you said something about a yoga blanket, what do you mean by yoga blanket? Or maybe you didn't
Tom Palizzi
Say I saw that. I saw that in the response as well. Speak
Melani Dizon:
That. Okay. I'm sorry. I'm not, not remembering that. For sleep satin fitted sheets. Yes. Satin fitted sheep. I said I sheep in sleeping satin fitted sheets help with movement. Yes. For sure. You just
Kristi LaMonica:
Recommend don't wear sat and pajamas with the sat and fitted she with
Melani Dizon:
The satin sheets. Right. It doesn't work out very well. Yeah. It's got experience. Yeah. We, for those of you who are interested in sleep, Sam just put up our primer on sleep, but we also just did a sleep Victory Summit on Friday. That was really interesting people experts that we had to talk about that. So, we'll have those recordings up soon. A couple of, no more. So, somebody said they've been on their meds for about three years, but recently have been dealing with pimples, itching, and rashes on their body. Has anybody had this issue, with medications that they can offer some help?
Robynn Moraites:
I haven't had it with regard to medication, but my body's first response to sort of any kind of a disruption is what we call an immunological response, AKA hives. And so, I have had a fair number of hives related to, to my Parkinson's one way or another. It's never been directly medication oriented, but I will say this, our bodies change with Parkinson's over time, and we come become more and more prone to an inflammation response. It could be something you're eating yeah. It might not be your meds. Right. And you can email me, and I'm happy to talk with you about it offline. I'll put my email in next to name. Thank you Robynn. Also yes, somebody asked about falling. We have a lot of resources about falling and ways to prevent falling. And we did a couple of great webinars this year about falling. So, Sam can throw those in the chat. We'll also make sure to conclude those in the show notes. Has anybody these are a little bit longer, but I do want to, I do want to mention this from Jan Grime. She's not able to be here today, but I thought her idea was so brilliant that I do want to tell you about it. So, she says, has anyone in this group ever heard of, or ever tried to have a group home for people living with Parkinson's I've been dreaming of such a thing for a small group of people who are basically independent but need a little help.
Melani Dizon:
They would have duties for the house and contribute what they can financially. It's just a dream because I know of people who have very little support, and they may be running out of funds at the same time. They're cognitively acute mm-hmm and totally with it. Has it ever been tried? Obviously, they would have to find other accommodations when the condition progresses to a certain point up to them, but it would be, they would be around to share with others. And I just like, isn't that perfect like that is, I love that idea so much, Heather apparently is showing us where this can happen. Right. Is that what you're doing? I love it.
You know what I don't actually I think there's a lot of things that like the Aspen Institute Legion institutes are doing with people with multigenerational and different housing situations. I don't think it's in no way. think it's coming. And I think that we're number one, we're learning that throwing people, aging people to the wolves is not okay. And there's a lot of things that are happening with just the aging population. So, aging and Parkinson's things are going to happen. And I think that having these ideas and having people that are interested in talking about them is only going to make it possible. And I do think someday that's, that's actually going to be a thing. So,
Kat Hill:
And sharing resources is, is, is very powerful. I think we're looking more at how to do that creatively, effectively supportively. And, and economically, because I think, you know, the biggest portion of the population is soon to be over 65. So, we're going to have to start getting creative as a society, not, you know, separate from people with Parkinson's so
Melani Dizon:
Right. And we move from like, you know, there's all levels of care, right? And there are some people with Parkinson's that are living alone, people that are aging living alone and whether they could or not don't want to be alone, want to have some people around that they can call and know that they're
Kat Hill:
Nearby. Amen. Amen.
Melani Dizon:
Okay. So, wow. We got through it all. I have more questions, but I know everyone's going to send some more. So, thank you all so much for being here today. Thank you for Doug and Christy and Brian, somewhere out in the world where he's not having the best internet access. Thank you so much for joining us today. And thank you
Kristi LaMonica:
So much for having me. I'm honored to be here. Like as best people in the world, you guys are.
Melani Dizon:
Well, we hope you come back. We hope you come didn't scare off. You
Kristi LaMonica:
Now love you all.
Melani Dizon:
We will we'll lives and the resources and the notes and anything that we dropped in here today. And thank you all for being here and we will look forward to seeing you in October. All right.
Tom Palizzi
See you. Thank you, buddy. Thank you very much. Good to share it with you
Melani Dizon:
Bye-bye.
To download the audio, click here.
Show Notes
We covered many topics in this month's Living with Parkinson's Meetup. Thank you so much to our panelists and participants for their great suggestions. Here are some of the key takeaways from the ones we discussed. While these show notes don't cover everything, we've included all the links we shared in our conversation, as well as other relevant links below.
Meet Our GUEST Panelists
We had one new regular and two guests on our panel this month! It's always great to have new faces and new perspectives in our Living with Parkinson's Meetup, and we hope you had a great time getting to know them. Here's a bit more information on each one:
Doug Reid - Regular Panel Member
Doug lives nearby the Davis Phinney Foundation in Lafayette, Colorado. He was diagnosed with Parkinson's at age 36 and has been struggling with the depression and motor symptoms that have come with it. During a particularly pivotal moment in his life, he decided to get Deep Brain Stimulation surgery due to a video the Davis Phinney Foundation published. While his symptoms have improved physically, he still suffers from loneliness and depression. That's part of what led him to become an Ambassador. He wanted to help others in his situation find a way to live well despite the changes and loss that come with a Parkinson's diagnosis. You can find out more about Doug's journey on his ambassador page.
Kristi LaMonica
Kristi hails from upstate New York and is one of our newer Ambassadors. While she was formally diagnosed in 2020, her career (as a scientist) has led her to believe symptoms were present as early as 2014. Her connection with the Davis Phinney Foundation came when she discovered our Every Victory Counts® Manual, which now resides under her coffee table for everyone to read. She started watching the Women with Parkinson's Council and knew she wanted to become involved with the Foundation. While she does not currently have an Ambassador page, look out for it being up soon so you can get in contact with Kristi and get to know her and her journey!
Brian Reedy
Brian is from Southern California in the Huntington Beach area. After a 2010 diagnosis, he suffered from limited mobility. However, this changed for him completely when he went to The Victory Summit Event in Las Vegas. Brian credits that event with changing his life. At the time, he was using a walker almost exclusively to get around, but after hearing about the value of exercise for people with Parkinson's, he found a physical therapist, which completely changed his quality of life. While he is currently regaining mobility from a recent car accident, his biggest joys are that he has learned that the more he moves, the better he feels. You can learn more about Brian on his ambassador page.
Ableism vs. enableism
As people with Parkinson's, there is no doubt that ableism is very present in day-to-day life. The definition of ableism is "discrimination in favor of able-bodied people" (via Oxford Languages). This can be people not hiring someone based on a disability, not providing accommodations, buildings without accessibility, and so on. However, there is a more sneaky type of ableism that our panelists talked about and that is enableism. Enableism is "the enablement of discrimination against disabled people" (via Deaf Child). This may show up when someone (maybe a care partner or other loved one) immediately cuts your food without asking if you would like that or doesn't invite you someplace because they aren't sure if there will be accommodations, even if you haven't asked for them.
One of the ways to combat enableism is to set clear boundaries. Our panelists suggested saying, "I understand that you want to help, but I need to be able to advocate for myself. Please ask before you do something for me." While this may seem like a no-brainer, our care partners or friends may get so used to helping with certain activities that they do it automatically, without asking if you actually need that help. Make sure that you don't let people (even extremely well-meaning people) take away your agency.
DYSKINETIC at the dentist
One of our audience members had a great question about how to handle dyskinesia at the dentist. While we didn't have the time to address it thoroughly during the session, Doug Reid followed up after the meetup with a great answer. Check out how he'd handle it below.
"If your dentist/hygienist isn’t already aware that you have Parkinson’s, I suggest you inform them before your appointment. Further, inform them that you experience dyskinesias, and so your appointment may take a little longer than a typical appointment.
For me, talking often made my dyskinesias worse. If you’re similar, at the start of the appointment, you may want to convey that info. Then, you can agree upon a “code“ to convey when you’re dyskinetic. For example, if you hold up your index finger, that means “I am dyskinetic, and I need a break.” An “OK” hand gesture, or a thumbs up, means “I’m good to proceed.”
Whenever I am feeling dyskinetic, I find that by relaxing (fortunately, in a dental chair, you’re already reclined!), closing my eyes, thinking calm thoughts (going to my “happy place”), and taking long, deep breaths (breathe in through the nose, and out through the mouth), often makes the dyskinesias go away, or at least subside a bit.
Finally, if you experience dyskinesia on a schedule, consider scheduling your appointment at a time you are the least dyskinetic. Since it’s important to take your medication(s) on a regular schedule, schedule your appointment around your medication schedule instead of the other way around. If you tell your dentist's office you have Parkinson's and that being able to come when you are ON will make things a lot easier, chances are they will do what they can to accommodate you."
Other Q&A
A few of the other questions we addressed, and you can find in the transcript and recordings, included:
- What are the rings/finger splints Kevin is wearing?
- Are there any cushions you can use to make sleep more comfortable?
- What do you do if you have restless leg syndrome to be more comfortable in bed?
- How do you know when it's time to stop driving?
- Why does it feel like my brain never turns off?
- Has anyone experienced acne, rashes, or itching due to medications?
Thanks for attending this webinar. we hope to see you again next month!
Mentioned Resources
- Ted Lasso "Be a Goldfish"
- How Long Can I Keep Driving if I Have Parkinson's?
- Who Created Rule 62?
- Mood and Parkinson's
- Advocating for Yourself as a Woman and a Person with Parkinson's
Additional resources
Missed this webinar? join us next time!
The Living with Parkinson's Meetup meets on the third Thursday of every month, and every session is recorded and shared for all to access. Register for the Living with Parkinson's Meetup here, after which you will be invited to join live and notified when a new webinar recording is posted. Are you interested in catching up on past Living with Parkinson's webinar recordings? You can find all recordings on various subjects on our Living with Parkinson's Youtube playlist, and don't forget to subscribe to our channel to be notified when new Youtube content becomes available.