Lewy Body Dementia: A Common Yet Underdiagnosed Dementia
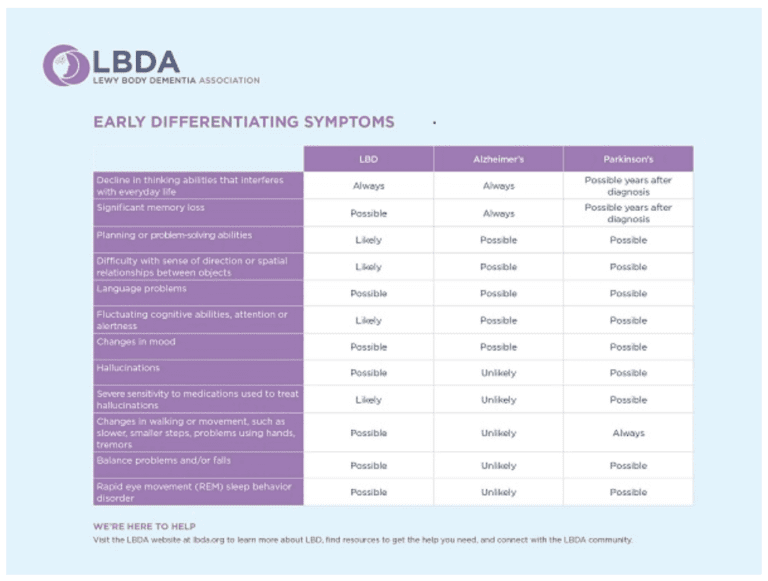
While it’s not a household word yet, Lewy body dementia (LBD) is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known disorders like Alzheimer’s disease and Parkinson’s, it is often underdiagnosed or misdiagnosed. In fact, many doctors or other medical professionals still are not familiar with LBD.
What is Lewy Body Dementia?
Lewy body dementia is not a single disorder but rather a spectrum of closely-related disorders involving disturbances of cognition, behavior, sleep, movement and autonomic function.
In these progressive disorders, Lewy bodies (abnormal deposits of a protein called alpha-synuclein) build up in the brain. Lewy bodies in the brain stem cause a disruption in the production of chemical messengers (neurotransmitters) called dopamine. Too little dopamine can cause parkinsonism, a clinical syndrome that’s characterized by tremor, bradykinesia (slow movement), rigidity and postural instability. Parkinsonism can be caused by Parkinson's disease itself as well as by other underlying neurological conditions such as LBD. These Lewy bodies are also found throughout other areas of the brain, including the cerebral cortex. The neurotransmitter acetylcholine is also depleted, causing disruption of perception, thinking and behavior.
A German neurologist, Friederich H. Lewy, first discovered the abnormal protein deposits (later named Lewy bodies) in the early 1900s as he was conducting research on Parkinson’s disease.
What’s the Difference Between Lewy Body Dementia, Parkinson’s Disease, and Alzheimer’s Disease?
Lewy body dementia is an umbrella term for two related clinical diagnoses: “dementia with Lewy bodies” and “Parkinson’s disease dementia.” These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending on where the Lewy bodies first form.
Dementia with Lewy bodies (DLB) is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a person’s ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first (or around the same time as parkinsonism) in DLB. The motor symptoms of Parkinson’s such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
In contrast, Parkinson’s disease dementia (PDD) is a term used for dementia that develops after a year or more of living with Parkinson’s, a disease that is caused by loss of dopamine-producing nerve cells. In nearly all cases of Parkinson’s, people experience motor symptoms in the early stages; some may also have very mild changes in cognition at diagnosis. Over time, non-motor symptoms of Parkinson’s may appear, including cognitive impairment, REM sleep disorder, memory problems, fatigue, anxiety, autonomic dysfunction, pain and more. Most importantly, not all people with Parkinson’s will develop dementia and at this time, it’s impossible to predict which individuals with Parkinson’s will also develop Parkinson’s disease dementia.
Finally, Alzheimer’s is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
Alzheimer’s disease is associated with a lack of acetylcholine, a neurotransmitter in both the peripheral nervous system (PNS) and central nervous system (CNS). Damage initially occurs in the hippocampus, a part of the brain that is involved in memory formation. Other portions of the brain, such as the temporal, parietal and frontal cortices, are progressively affected in those with Alzheimer’s disease.
In comparison, people with dementia with Lewy bodies (DLB) may first present with REM sleep behavior disorder years or even decades before developing dementia, or they may experience visual hallucinations early in the course of their dementia. These are features that help differentiate DLB from Alzheimer’s, even in the early stage of dementia.
What Causes Lewy Body Dementia?
The causes of LBD are not yet well understood, but research is ongoing in this area. There are probably multiple factors involved, including genetic and environmental risk factors that combine with natural aging processes to make someone susceptible to LBD.
For more information, visit www.lbda.org.
Modified with permission from the Lewy Body Dementia Association
To learn more about motor symptoms related to Parkinson's, visit here.
To learn more about non-motor symptoms related to Parkinson's, visit here.















I had never heard of lewy bodies dementhia until my wife gor it. We need to do more research on it and provide more information to the public.
Thanks for commenting, Larry. We hope that by creating content on the topic, our community will become more informed and fewer people will be misdiagnosed.
It is my understanding that not all Lewy body patients develop Parkinson’s, but that if an autopsy of a Parkinson’s brain does not show Lewy bodies, then it wasn’t Parkinson’s.
Hi Elaine – I’m not sure if that’s the case; however, you may be able to find some answers about that from the LBDA. Here’s an article on their site that includes questions from caregivers that may be of interest to you: https://www.lbda.org/go/caregiver-faq.
There seems to be greater confusion between Lewy Body Dementia and Parkinson’s Disease due to tv ads (the other side of Parkinson’s). Here recently Alan Alda said he decided to get tested for Parkinson’s due to “cutting edge” research suggesting REM sleep disturbances tend to be precursors to Parkinson’s. However, as in the article above mentions REM sleep disturbances have long been known as a key early sign of Lewy Body Dimentia. Is this confusion due to doctors lack of knowledge about Lewy Body Dementia, confusion in the terminology or a struggle for funding?
As a former caregiver of someone with Lewy Bodies it’s disturbing to see such confusion. There seemed to have been a ray of light from Robin William’s wife for educating the medical establishment. I remember doing my own research to figure out what was wrong with my loved one in a medical text book. There was a whole chapter on Alzheimer’s, seven pages on Parkinson’s disease and only three paragraphs on Lewy Body.
Hi Clay,
Thank you for your comment. There is a lot of confusion and TV ads never seem to clear it up, as you suggest. I also think that this could very well be confusion on the part of doctors about Lewy Body Dementia as well. The reality is, there are many doctors who end up treating people with LBD, PD and AD and they are not specialists. They are GPs and for better or worse, they are the person’s only option for care where they live. The doctors do the best they can but these are very complicated diseases and even specialists sometimes struggle to parse out all of the symptoms. The other challenge and is that everyone with Parkinson’s presents differently and the timing of certain symptoms has an impact on diagnosis and treatment. You’re not alone in thinking this way, and it’s one of the reasons we wanted to write about it. People were searching for Lewy Body Dementia on our site, and we wanted to create content to help distinguish between these three diseases. And also let people know that there is a great association, the Lewy Body Dementia Association to look to for more information. Hopefully calling attention to the confusion will continue to keep the conversation top of mind.
I was wondering if anyone is doing research on the genetic implications of having one parent with Alzheimer disease and the other with Parkinson’s.
I have one daughter with MS as well. Seems to me that they could all be related either genetically or environmentally.
That is interesting, Theresa. I don’t know of any specific research where all three of these conditions are being studied and compared. There’s a great deal of research happening right now around the relationship of gut health to neurological disorders. You may find these resources interesting if you haven’t already seen them.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4892191/
https://neurosciencenews.com/gut-neurological-diseases-9065/
https://jamanetwork.com/journals/jamaneurology/article-abstract/2661302
https://www.michaeljfox.org/understanding-parkinsons/webinar-registration.php?id=37&e=1623818&k=32A45B9968329E31525CDD93A2EB2B48
At first my husband was diagnose with PD about 4 months ago but after researching on what I saw everyday that the doctors did not see, I knew that something else was going on. Yes he had memory loss unstable when walking and shaking . Why could he not step up on curb or not speak or hold his silverware to eat ? These symptoms may only last 30 minutes to a hour at a time it did not make since to me, so I kept after doctors. Would take him in to doctors office when it was happening a lot of the time even though it might be over before we got there. It became very overwhelming on my part and frustrating I started keeping notes of what was going on with him, times, symptoms how long it went on and thats when we got a true diagnosis LBD with PD. He has started medications and is much better we are taking each day at a time even though symptoms come up like just this morning I came back from store and he could not speak . He was pointing to his mouth and shaking his head. I knew right away so just explained it was the LBD , poke some fun at him told him he could not give me hell for going to store. lol . I made coffee and began telling him about my trip to store after awhile he was able to make some noises soon after we were talking just like nothing happen. It is my advice to anyone reading this , research and keep notes it can really help doctors give a true diagnose .
Thank you for sharing your story, Carol. It sounds like your husband has an amazing care partner in you. I love that the two of you have found a way to bring some levity to a very serious and life-changing situation. I’m sure others will find a great deal of inspiration (and some great ideas) from what you’ve shared. Every victory counts!
My father had Lewy Body dementia that was mistaken for Alzheimer’s until very late in his life. I’m 71 years old and I’ve recently self-diagnosed as being in the early stages of LBD with symptoms like REM sleep disorder, unstable heart beat and blood pressure, difficulty swallowing, etc. Luckily, I don’t yet have noticeable cognitive or motor symptoms. I owe a lot to the diagnosis of my father and resources available on the Internet. I’m scheduled to see a neurologist soon. In the meantime, my wife is doing research to get our affairs in order and to prepare to become my caregiver. At least we have a chance to prepare for what we know is coming. Hopefully, in the future, more early-stage LBD sufferers will have the same opportunity.
Thank you for reading, James. I’m sorry that you’re going through this. It sounds like you are on top of it, and your wife is ready to take on the role of care partner. Please let us know if there’s anything we can do to support you in the future. If you ever feel like sharing your story with us, we’d love to hear more about it. You can do so by completing the form here: https://www.davisphinneyfoundation.org/get-involved/moments-of-victory/. All the best to you and your wife.
My husband was diagnosed with PD 7 years ago but suffered rem sleep symptoms for years prior to diagnosis His symptoms are now much more severe eg.Postural Hypo-tension lack of concentration, inability to perform everyday tasks like brushing teeth, putting on his glasses etc etc.
This confusion only lasts 30 mins or so but becoming more frequent.
Definitely PDD.
Must look at meds list.
Your article has been very informative & helpful. Thankyou.
Hi Mary – Thank you for reading. I’m sorry you and your husband are going through this, but I’m glad this article was helpful to you. Wishing you both the best.
Just received confirmed diagnosis today regarding my husband symptoms , that he has been having for the last two years. Lewy Bodies Dementia. He had a DAT scan. He has textbook symptoms. I am reading everything I can to help us get through this. I am his care partner, and the V.A. Is his provider, the team is wonderful and supportive, he has a G.P. psychiatrist, Neurologist, Social worker counselor for both of us, a social worker when we are ready, I feel supported and ready to tackle our future. Look forward to ready all I can from your site. Thank you
Thank you for reading, Terry. I’m sorry you and your husband are going through this. I hope you will find education, hope and inspiration within our community. If there’s anything we can do or information we can provide, feel free to reach out.
My 88 yr old husband has ARMD and 12 months ago started hallucinating.He was diagnosed with Charles Bonnet Syndrome and prescribed Seropia tabs 50 mgm daily and Exelipatches,9.5mg ,They are not making a lot of difference to the hallucinations and mood swings ,He had an MRI of the brain 6 weeks ago and he has now been diagnosed with Lewy Body Zander are awaiting an app to discuss his care with the specialist I have had a very stressful couple of months and feel this could have been avoided if he had the diagnosis sooner ,any advice from Carers of people suffering from L B D would be appreciated
Hi Margaret – I’m so sorry to hear you and your husband are going through this. Our community members often share how stressful and upsetting a delayed diagnosis process is. Have you looked into LBD or Parkinson’s support groups in your area? Many are mixed groups and many communities have ones especially for care partners. These might be a great place for you to find others who are traveling a similar path.
I was reading through your comments and Theresa’s comment struck me…My mother (73) has PCA/Benson’s Syndrome…Her younger brother (70)was just diagnosed with LBD…Her father had Parkinson’s (died at 79 ) and her mother had late (old age? not diagnosed but obvious, died last year @ 91) dementia… her oldest brother and sister do not show any symptoms however they moved out before the family moved to Ft. Myers, Fl…. the oldest sister stayed in Miami(came down with MS, died 3 years ago from complications) the oldest brother went to collage and then military, he is fine. The youngest sister (65) is not showing symptoms that are concerning to Dr.’s as of yet… and I (53) lived in the Ft.myers home with my mother until I was 6. which leads me to my point… everyone who lived in this Ft. Myers home has suffered from some form of these LBD/PDD … diagnosed around the age of 70ish. I’m concerned because My aunt who had MS, we believe it was environmental as we have studied clusters of MS in Miami and the Florida Keys. What I find frightening is the commonality of family diseases of those who lived in the Ft. Myers home. I am concerned that this may have been environmental also and with the lack of research on this type diseases cause we will probably never know for sure. My Aunt and I feel like ticking time bombs, waiting for the timer to expire…
Dear DeAnn,
I’m so sorry to hear about all of the people in your family who have been living with these diseases. There are definitely people investigating environmental relationships. Here’s an article you might want to check out.
My husband was diagnosed with Parkinson’s in Oct. 2016. Jan. 2017 doctor in Mayo Clinic diagnosed him with Levy Body given medications that helped except for hallucinations and terrible dreams kicking and throwing arms especially at night needed our adult children took turns staying at night until May 2017 when we went back to Mayo he did one change of meds and within 3 nights I was able to stay alone with him no hallucinations. He still has occasional dreams some happy dreams very seldom wild dreams. Usually prop a pillow behind his back so he lays on his side then no dreams. He walks with a cane was walking with a walker. He occasionally sees things like animals or people in our yard not as often but occasionally. He visits well with our friends just a different person then the first 6 months of 2017. He does have hallucinations in his mouth occasionally like lots of loose teeth but then he can finally say he is just having hallucinations.
Hi Phyllis – Thank you for reading. I’m very sorry you and your husband are going through this. Perhaps this article may be helpful for you: https://www.davisphinneyfoundation.org/blog/how-to-bring-light-to-the-darker-side-of-parkinsons-a-primer-on-hallucinations-and-delusions-and-how-to-manage-them/
My husband was diagnosed last August with Parkinson’s with dementia. The diagnosis does not call it LBD; however, everything I’ve read said if dementia was diagnosed at the same time as Parkinson’s it was LBD. Is that correct? My husband has significant short term memory loss, visual perception problems, paranoia, REM sleep disturbances, restless leg, balance problems, gait problems, and some confusion. He also has significant hearing loss and will not wear his hearing aid. His brother has severe MS which was finally diagnosed by the VA about 7-8 years ago. He had symptoms for 10 years but could not get an MRI through the VA and he had no insurance. My husband also has a autoimmune disease called Shjorens Disease with symptoms similar to Rheumatoid Arthritis. Interested to know if there’s a connection? Also. wondering about the prognosis and stages so we can do some better planning. Thank you!
Hi Paulette,
Thank you for reading. I’m very sorry about your husband. In terms of Shjorens Disease and its connection to Parkinson’s, this article/study may be helpful in understanding it: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5509109
In terms of prognosis and stages of Parkinson’s, it truly is a case by case basis. So much depends on dominant symptoms, age at diagnoses, comorbidity, quality of life and more. I highly recommend that you register for our upcoming webinar with Dr. Daniel Weintraub on September 11th. (Registration for that will be open next week.) He will be talking about psychiatric and cognitive complications in Parkinson’s as well as Parkinson’s progression. You can stay up to date on all of our upcoming webinars and register for them here: https://www.davisphinneyfoundation.org/resources/webinars. Best wishes.
My mom was diagnosed with Lewy Bodies about three yrs ago. The hallucinations seem to be the worst! To the point where she physically hurts herself. We have discussed with her neurologist but there doesn’t seem to be anything they can do. It was a long hard road to get the correct diagnosis but now I feel like it really hasn’t helped. Is there any kind of medication she can take to help with the hallucinations?
I am so sorry you and your mom are going through this. Unfortunately, if your neurologist hasn’t offered any solutions, we wouldn’t be able to either. Does your mom see a Movement Disorder Specialist? A doctor that specializes in movement disorders like Parkinson’s will likely have some recommendations about medication options she may be able to try. In the meantime, this article may be helpful to you: https://www.davisphinneyfoundation.org/blog/how-to-bring-light-to-the-darker-side-of-parkinsons-a-primer-on-hallucinations-and-delusions-and-how-to-manage-them/